This blog is based on an original research article. The views expressed are those of the author(s) and reviewer(s) at the time of publication.

Rebecca Whybrow, Lecturer in Midwifery at King’s College London, is an experienced midwife and researcher. She specialises in high-risk pregnancies, shared decision-making and health service policy. In this blog, she describes her recent research which aims to improve shared decision-making for pregnant women.
We developed an aid to shared decision-making for pregnant women with high blood pressure (hypertension). When the aid was used in consultations:
- women’s uncertainty about taking antihypertensives was reduced
- more women intended to take their medication as prescribed.
National guidelines recommend that pregnant women with high blood pressure are treated with medication (antihypertensives). But hospitals in England vary in the treatment they offer. Women themselves are concerned about the safety of antihypertensives; they may experience internal conflict as they balance their own health needs with those of their unborn child. As a result, many do not take their treatment as prescribed.
Shared decision-making is often used in healthcare where there is uncertainty about the best approach. However, it is not routinely used in the management of blood pressure in pregnant women. We worked with women and healthcare professionals to codesign an aid to shared decision-making. Together, we developed infographics for professionals to share with women during consultations.
Some of the infographics show the benefits and potential harms of treatment – both to the pregnant woman and her baby. Others give information about the specific drugs recommended in the UK for this group of women. An example of the infographics is below:
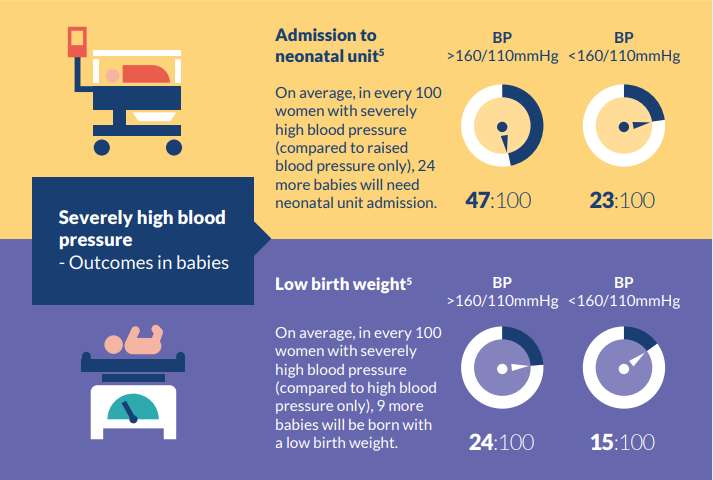
Severely high blood pressure – Outcomes in babies
Admission to neonatal unit
- BP >160/110mmHg, 47:100
- BP <160/110mmHg, 23:100
On average, in every 100 women with severly high blood pressure (compared to raised blood pressure only), 24 more babies will need neonatal unit admission.
Low birth weight
- BP >160/110mmHg, 24:100
- BP <160/110mmHg, 15:100
On average, in every 100 women with severely high blood pressure (compared to high blood pressure only), 9 more babies will be born with low birth weight.
Our study found that, when the infographics were used in consultations with pregnant women with high blood pressure, they felt less conflicted about taking antihypertensives. More of the women said they intended to take the treatment as prescribed.
The infographics enabled women with lower literacy levels, and those whose first language was not English, to engage in shared decision-making.
Co-designing the decision aid
Our aim was to develop an aid that was acceptable to women, and made shared decision-making easier for healthcare professionals.
The questions that guided its development were:
- What are the key decisions for pregnant women with high blood pressure?
- What information would help women take part in decision-making?
- What are the main benefits, and the potential harms, of treatment – to women and to their unborn child?
Our steering group and focus groups included midwives, obstetricians, physicians, and pharmacists, as well as women with lived experience. Almost half of the women in our study were from Black and South Asian communities. High blood pressure in pregnancy is more common in these communities, and women are up to 4 times more at risk of dying than White women.
We worked with health design experts to refine the aids until the steering group was satisfied. The steering group tested the infographics in antenatal appointments to make sure they were usable.
We then implemented the shared decision-making aid in 3 NHS Trusts. Among pregnant women with high blood pressure, using the aid reduced women’s uncertainty about taking antihypertensives. Many more intended to take the treatment as prescribed.
The aid was acceptable to women and professionals alike. The length of consultations was a concern for healthcare professionals. But they reported that the in-consultation infographics supported shared decision-making. One said: “I love the infographics I use them in my antenatal clinic all the time now”.
What we learnt from our partners
Collaboration and consultation were at the heart of this project and key to its success .
In developing the aid, observing consultants with experience of the condition and of shared decision-making enabled us to map what high-quality shared decision-making looked like. Similarly, observing less-experienced professionals highlighted areas for improvement.
Interviews and focus groups with healthcare professionals and women with lived experience ensured the aids would be acceptable and feasible.
Working with health communications experts, along with experts in shared decision-making, resulted in innovative infographics.
The development of the decision aid was guided by our charity partner Action on Pre-Eclampsia, which hosts the decision aid on its website (to date, there have been almost 5000 unique visitors to the webpage, and more than 3000 downloads).
We aligned the aids with NICE guidance and sought NICE endorsement.
What’s next?
Aids that are used during consultations to increase shared decision-making aids are a step towards more personalised care. The approach we took could be adopted for a variety of decisions in pregnancy and across healthcare. We plan to develop further pregnancy-related decision aids for use during consultations. We will be investigating their impact on evidenced-based decision-making and pregnancy outcomes.
We recommend others consider innovative approaches to personalised decision-making during consultations.
You may be interested to read
This Blog is based on original research: Whybrow R and others. Implementation of a novel shared decision-making intervention in women with chronic hypertension in pregnancy: multiple-site multiple-method investigation. Pregnancy Hypertension: An International Journal of Women's Cardiovascular Health 2022;30:137-144.
Funding: This work was supported by the NIHR and by the NIHR Collaboration for Leadership in Applied Health Research and Care South London (NIHR CLAHRC South London) at King’s College Hospital NHS Foundation Trust. The NIHR Applied Research Collaboration (ARC) South London has since replaced the NIHR CLAHRC South London.
Conflicts of Interest: None declared.
Disclaimer: Summaries on NIHR Evidence are not a substitute for professional medical advice. They provide information about research which is funded or supported by the NIHR. Please note that the views expressed are those of the author(s) and reviewer(s) at the time of publication. They do not necessarily reflect the views of the NHS, the NIHR or the Department of Health and Social Care.