This Collection brings together 5 examples from research that could reduce the need for surgery. They highlight less invasive options with reduced risks that give some patients similar or better outcomes. The findings support decision making, and offer value for money for the NHS. The information will be useful for policymakers and those commissioning and delivering services.
The NHS waiting list in England for consultant-led hospital treatment (diagnosis, surgery or another treatment) stands at 7.6 million (August 2024). The biggest waiting list, at over 850,000, is to see a specialist in trauma and orthopaedics, for a hip or knee replacement for example. While people wait, they are often in pain and their condition may deteriorate.
Reducing these waiting lists is a challenge for the NHS with no simple answer. An NIHR-funded report described a combination of activities that increase the supply and manage the demand for healthcare. Recent evidence from The Health Foundation has shown the potential of NHS surgical hubs to reduce waiting lists for surgery.
Another strategy to free up operating theatres, staff time, and other surgical resources is to consider whether surgery is the best option for patients. Strong NIHR research has shown that non-surgical alternatives (including watch and wait), can offer similar or better outcomes, but with fewer risks or side effects, and may be a better choice for some people.
NHS policymakers, commissioners, managers and clinicians could consider that:
- a watch and wait approach reduces the need for surgery among people with uncomplicated symptomatic gallstones
- one-stage is as good as 2-stage surgery to replace infected artificial hips
- opting for active monitoring of low or intermediate-risk localised prostate cancer has the same high survival rates as surgery or radiotherapy after 15 years, and avoids the side effects of radical treatment for many men
- non-surgical approaches give better outcomes than emergency surgery for people with severe frailty admitted to hospital with severe gut problems
- a plaster cast is as good as surgery for a broken scaphoid bone in the wrist
A watch and wait approach reduces the need for surgery among people with uncomplicated symptomatic gallstones
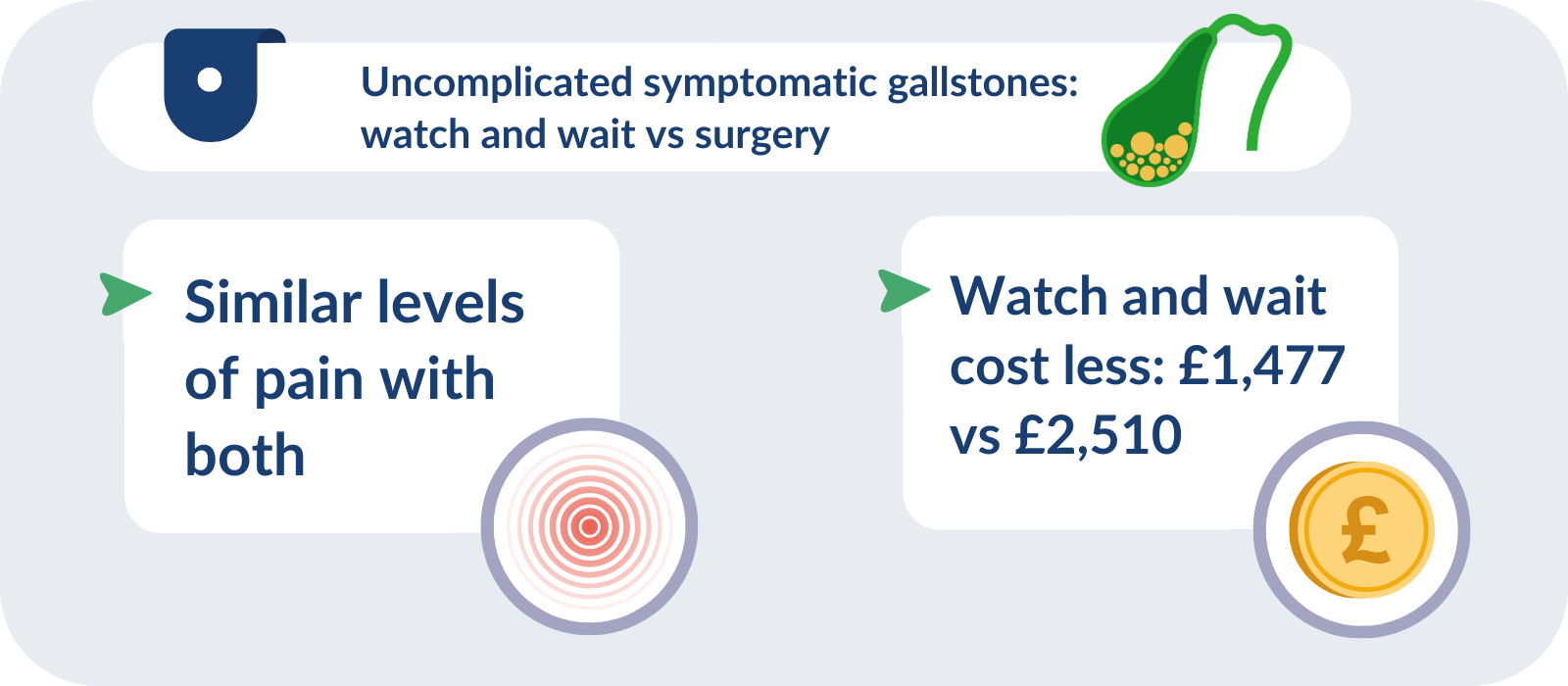
Gallstones are small stones that form in the gallbladder. They do not usually cause symptoms or need to be treated. If they become trapped, however, they can cause severe abdominal pain. Standard treatment for symptomatic gallstones is laparoscopic (keyhole) surgery to remove the gallbladder (cholecystectomy). This surgery is common; more than 60,000 cholecystectomies were performed in England in 2018/19, at a cost of around £200 million to the NHS.
However, surgery carries its own risks and some people continue to experience symptoms afterwards, for reasons that remain unclear. An alternative approach is to adopt a ‘watch and wait’ strategy before operating to see if pain resolves.
A randomised trial (C-GALL) involved 434 adults with uncomplicated symptomatic gallstones (gallstones that caused pain but not more serious problems such as jaundice). Half the participants were in the surgery group; half in the watch and wait group (painkillers when needed and advice on steps to take if symptoms flare up). If symptoms became too severe, those in the watch and wait group could opt for surgery to prevent and treat further pain. The research compared the outcomes of both groups.
The study found that after 18 months, pain was the same in both groups. Most (67%) people in the surgery group had received surgery; most of the others had refused surgery, or were on a waiting list. Some (25%) in the watch and wait group had surgery; but most neither had surgery nor were waiting for it.
Watch and wait cost less (£1,477 per patient) than surgery (£2,510 per patient, based on NHS costs, 2019/20). There was no difference in quality of life over 24 months from when people started the study, meaning watch and wait was highly likely to be cost-effective.
The findings could support shared decision-making between clinicians and people with uncomplicated symptomatic gallstones. Performing fewer surgeries for gallstones could avoid the associated risks for many people, provide a similar outcome, and save NHS resources. The findings are beginning to influence practice, the researchers say, and allow people to opt for watch and wait rather than being listed for surgery immediately.
One-stage surgery is as good as 2-stage surgery to replace infected artificial hips
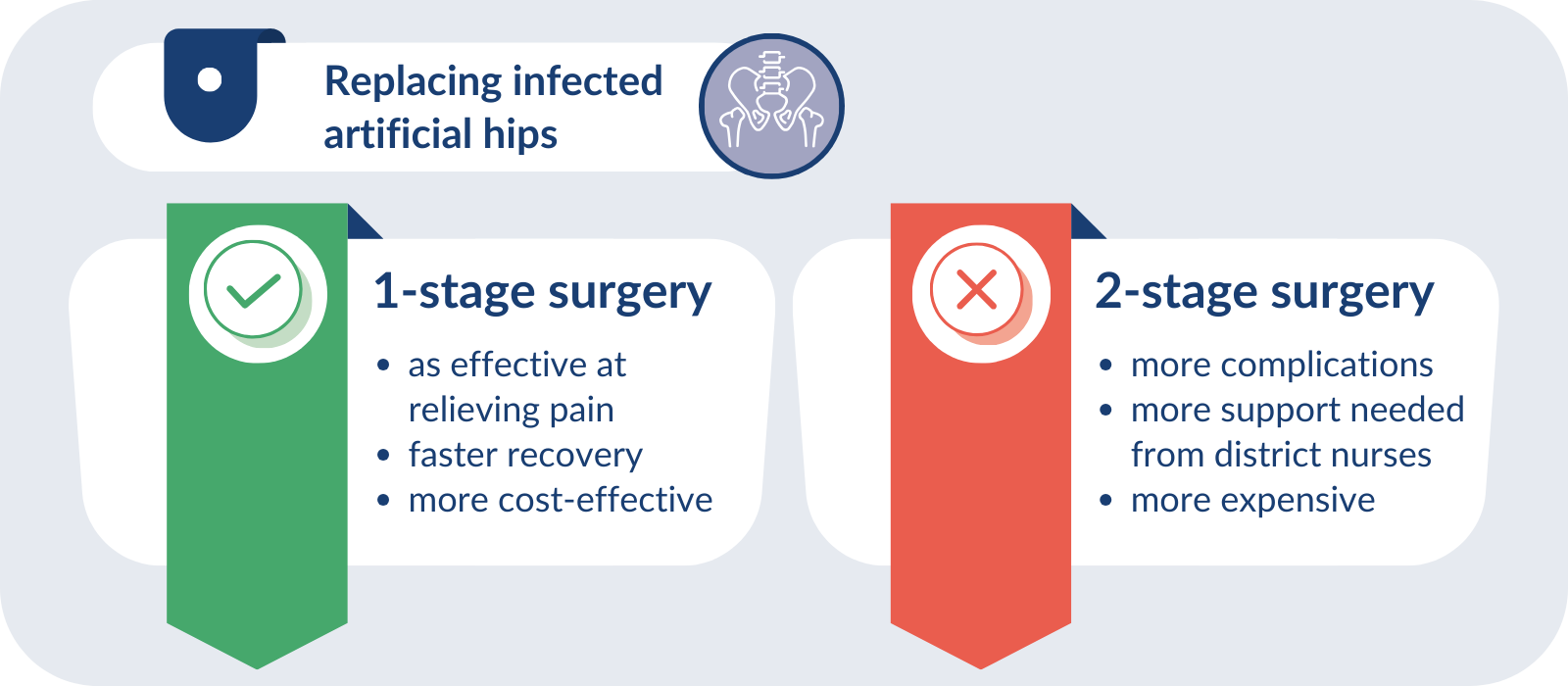
Hip replacements are carried out to treat pain and stiffness most commonly caused by osteoarthritis. This is a common procedure; in 2022, more than 100,000 people in England, Wales and Northern Ireland had a first hip replacement. Most people recover well afterwards, but some develop an infection in the artificial joint (1–2 people for every 100 who have a hip replacement).
Infection can cause severe pain or disability. People may need surgery to remove their artificial hip and the infected tissue, and replace the artificial joint. This can be carried out in one or 2 surgeries. The 2-stage approach allows surgeons to ensure, as far as possible, that the infection is gone before they implant a new joint. But this can delay the replacement of the joint for weeks or months. A one-stage surgical approach, in which infected tissue and implants are removed, and the new joint inserted in a single operation, is also available.
A randomised trial (INFORM), involved 138 adults requiring surgery to replace an artificial hip after infection. The research compared how well people recovered from the different surgical approaches.
The study found that, after 18 months, one-stage surgery was as effective as a 2-stage approach at relieving pain and improving hip stiffness and function (ability to carry out everyday activities). One-stage operations resulted in fewer complications during surgery, patients recovered more quickly, and it was more cost-effective (a benefit of over £11,000 for healthcare and personal social services based on UK costs, 2018/19). People who underwent 2-stage surgery required more support from district nurses and home care workers.
One-stage surgery is not always feasible, but the researchers recommend its use whenever possible. The team worked with expert stakeholders to produce best practice guidelines based on their results. The implementation of the guidelines could improve treatment pathways and care nationally, the researchers say.
Opting for active monitoring of low or intermediate-risk localised prostate cancer has the same high survival rates as surgery or radiotherapy after 15 years, and avoids the side effects of radical treatment for many men
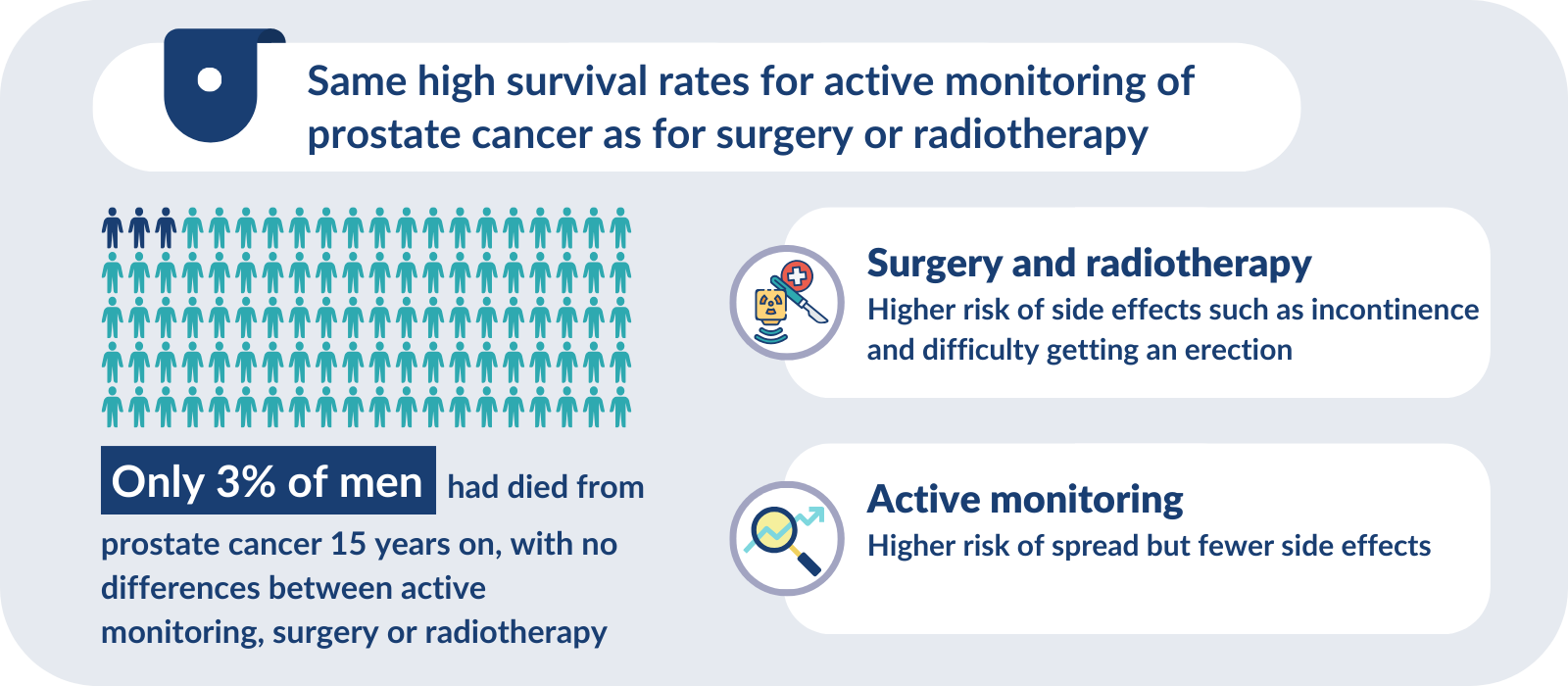
Prostate cancer is the most common cancer in men, with more than 55,000 new diagnoses each year in the UK. While some localised cancers (confined to the prostate) will become harmful and need treatment, most grow slowly, or not all, and may not cause any problems or reduce life expectancy. It is difficult to predict reliably whether and how the cancer will grow.
The conventional radical treatments for localised prostate cancer are surgery or radiotherapy. These treatments carry side effects, including leakage of urine or faeces (incontinence) and difficulty getting an erection. An alternative treatment option is active monitoring, which involves regular blood tests, clinical examinations, scans and sometimes biopsies, with radical treatment offered only if the cancer progresses. A long-running randomised trial (ProtecT) involved 1,643 men with localised prostate cancer. It compared the 3 treatment approaches: active monitoring, surgery and radiotherapy. Long-term follow-up has recently been published.
15 years after diagnosis, 3% of men had died from prostate cancer, with no differences between treatment approaches. The risk that the cancer had spread outside the prostate was low in all 3 groups, but was reduced by half in men who had radical treatment (surgery or radiotherapy) compared to active monitoring (5% versus 9%). After 15 years, 1 in 4 men in the active monitoring group (24%) had not needed surgery, radiotherapy or any other prostate cancer treatment and were spared the negative side effects.
Overall quality of life was similar in all treatment groups, but each had different side effects. For example, over 12 years, men in the surgery group were more likely to have urine leakage and difficulty getting an erection, whereas leakage of faeces was more likely in the radiotherapy group.
Over 10 years, NHS costs were lower for active monitoring (£5,913) than radiotherapy (£7,361) and surgery (£7,519, based on NHS costs, 2014/15). Active monitoring was the most likely cost-effective option for younger men, radiotherapy for older men. More follow-up is needed to find out which treatment is most cost-effective over a man’s lifetime.
Earlier findings from the same study have already changed practice through updated NICE guidance (2021). These additional long-term outcomes give individual men and clinicians more information on which to base the decision on the best approach to manage localised prostate cancer. Men need to weigh up the trade-offs between possible benefits in cancer control with surgery and radiotherapy, and a higher risk of spread, but fewer side effects with active monitoring, in the context of high survival rates, to enable well-informed treatment decisions.
Alternatives to emergency surgery are better for people with severe frailty admitted to hospital with acute gut problems
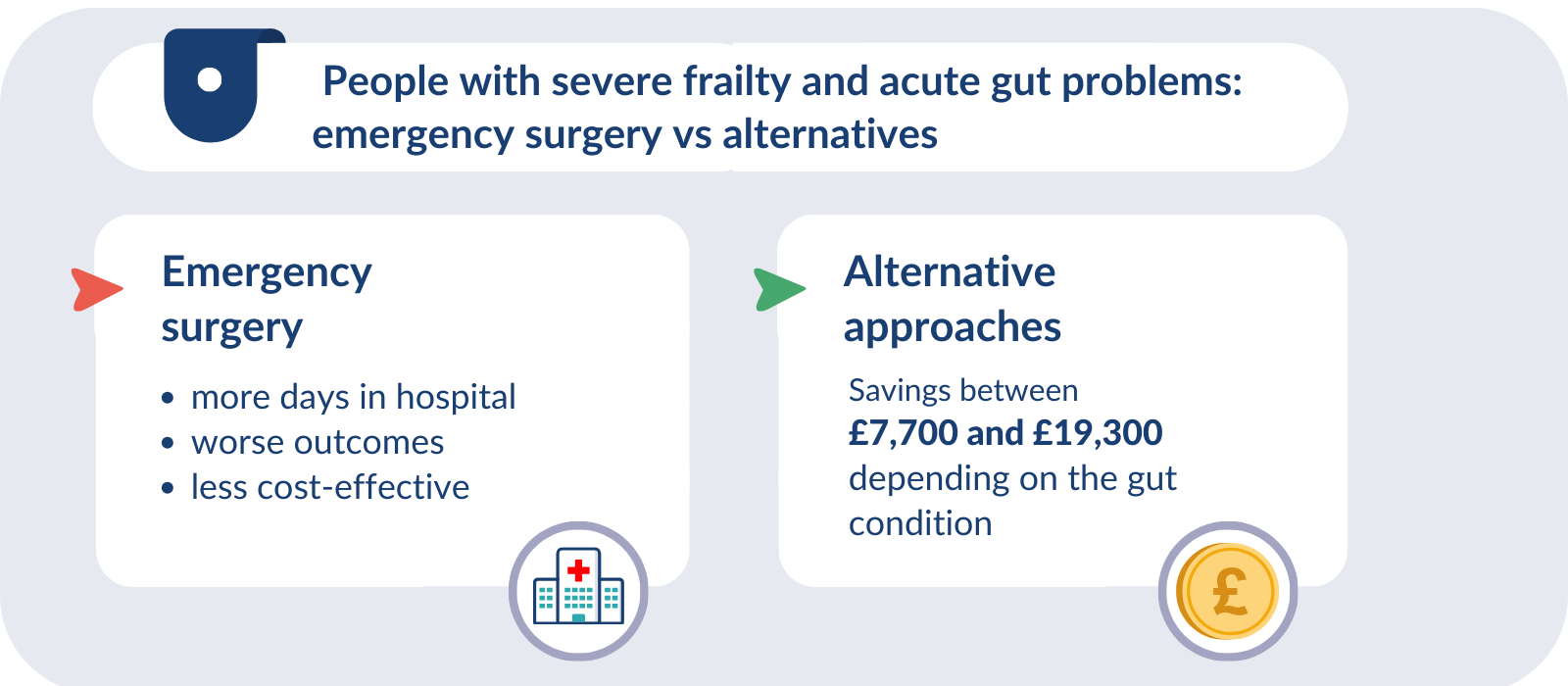
Large numbers of people with digestive (gut) conditions that start suddenly, such as acute appendicitis and abdominal wall hernia, are admitted to hospital as an emergency. Many people have surgery; around 50,000 emergency appendectomies are carried out each year in the UK, for example. Other people will be treated with alternative, non-emergency surgery approaches, such as medicines, non-surgical procedures such as drainage of an abscess, or later surgery. Hospitals vary considerably in their use of emergency surgery versus alternative approaches.
Recent research (the ESORT study) was based on more than 887,000 patient records of people with 5 common acute gut conditions: diverticular disease (inflamed pockets in the lining of the bowel), cholelithiasis (swelling of the gallbladder), appendicitis, abdominal wall hernia and blocked bowel. The study explored whether emergency surgery improves outcomes or is more cost-effective than other approaches to care. It looked at the cost-effectiveness of emergency surgery compared to alternatives for different subgroups of patients, including according to their level of frailty before the emergency admission.
Overall, for each condition, emergency surgery was not more effective or cost-effective than other approaches. For people with severe frailty (data from over 27,000 patient records across the 5 conditions), outcomes were worse following emergency surgery than alternative approaches. Patients were in hospital for more days (between 6 and 39 more days depending on the gut condition) within the 3-month follow-up period if they had emergency surgery rather than alternative approaches, and emergency surgery was not cost-effective. Depending on the condition, the average costs at 1 year were between £7700 and £19,300 (2019/20 prices) lower with alternative approaches to emergency surgery compared to emergency surgery.
For people with severe frailty, outcomes may be better and average costs lower if alternative approaches to emergency surgery are used. The findings emphasise the need for frailty assessments as part of preoperative checks for emergency admissions for acute conditions. The researchers say these assessments could identify people who would benefit more from alternative approaches to emergency surgery which include drug treatment, non-surgical procedures or later surgery.
Plaster cast is as good as surgery for a broken scaphoid bone in the wrist
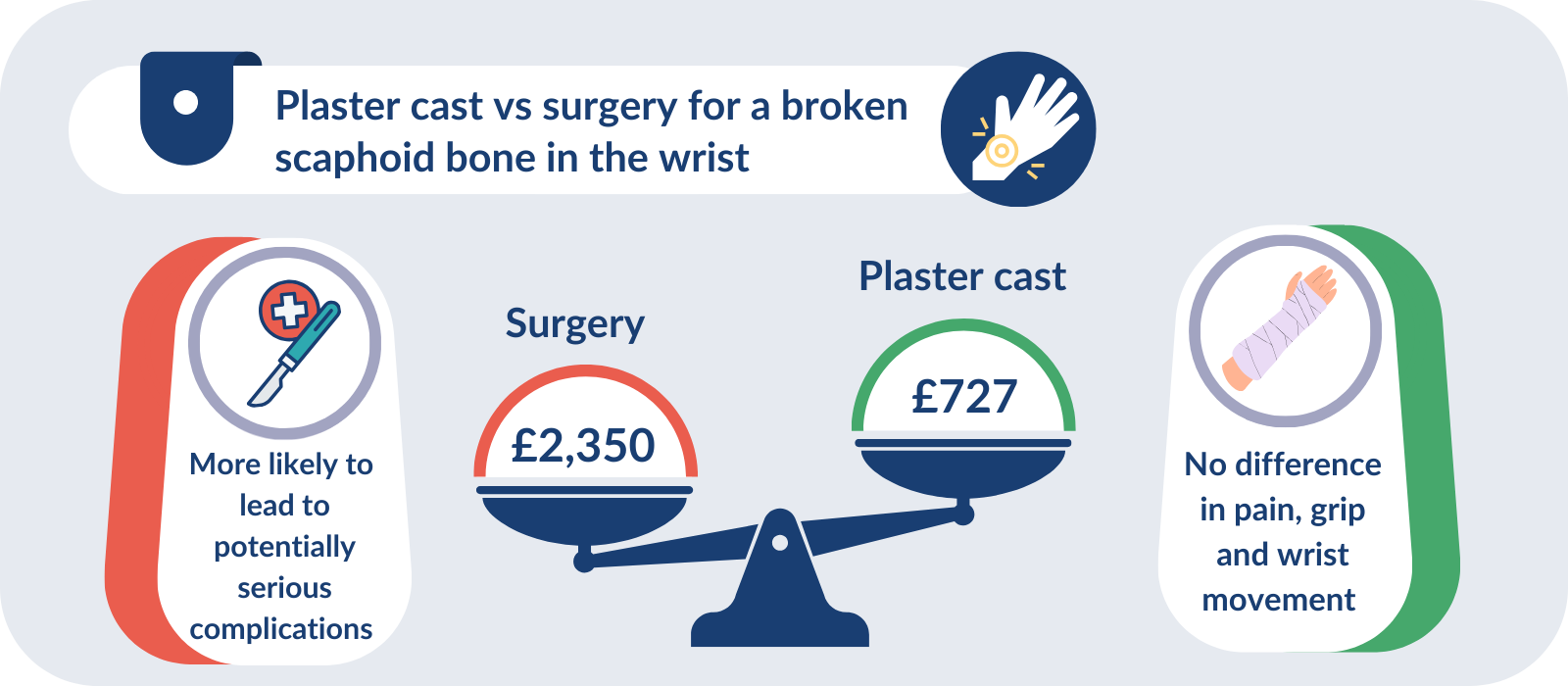
Fractures of the scaphoid bone in the wrist occur most commonly in younger men; they are usually the result of a fall onto an outstretched hand. It has been estimated that around 7,200 fractures are diagnosed each year. They are a significant public health problem as they affect people in their most productive working years. A broken scaphoid bone is usually a straightforward injury. But if it does not heal normally, arthritis usually develops in the wrist.
Traditionally, scaphoid fractures were treated by immobilising the wrist in a plaster cast. The last two decades, however, saw an increasing trend to perform surgery to fix the injury, by putting a small screw across the break. This was despite the lack of good evidence that surgery led to better outcomes. A high quality trial (SWIFFT) comparing the 2 approaches has provided much needed clarity.
The study involved 439 mostly male (83%) participants with a confirmed scaphoid fracture displaced by 2 mm or less. It found that plaster casts are just as effective as surgery. After 1 year, there was no significant difference in wrist pain, grip or wrist movement between the two groups. There was also no difference in the number of days absent from work due to the wrist injury. Surgery was more likely to lead to potentially serious complications, such as infection and nerve complications, and costs to the NHS were significantly higher. For each patient, over 1 year, surgery cost £2,350 compared with £727 for plaster cast treatment, based on 2017/18 costs.
The researchers have continued to follow the progress of the patients. New findings have shown that after 5 years there are still no important differences between wrist pain, grip or wrist movement between the two groups.
The research suggests that by opting for a plaster cast, patients can avoid the risk of surgery, while hospitals can keep service delivery simple and cost effective, without compromising patient outcomes. The study has influenced practice standards and has had an immediate impact. Even during the trial, the researchers say there was a shift away from surgery to simply treating with a plaster cast.
Conclusion
This Collection brings together examples from research showing that, for a range of conditions, surgery is not always necessary, nor the best option. Non-invasive alternatives can produce similar or better outcomes for patients, avoid the risks associated with surgery and save money for the NHS.
This evidence will support shared decision making between individuals and clinicians when considering the most appropriate approach. It will allow people to consider the benefits and harms of the options available, alongside outcomes that are important to them. People with uncomplicated gallstones may prefer to avoid surgery and instead choose a watch and wait approach. Men with localised prostate cancer may opt for active monitoring to reduce the likelihood of the side effects of radical treatment.
The research shows that surgery can even result in poorer outcomes. People with severe frailty had worse outcomes after emergency surgery for gut problems; alternative approaches would be better. And 2-stage surgery rather than a single procedure to replace infected artificial hips led to more complications and slower recovery.
Our 5 examples provide evidence that delaying, reducing or avoiding surgery altogether can be the best approach for some patients; it can indeed optimise their care. At the same time, non-surgical approaches release valuable operating theatre and staff time, and free up surgical resources. Patients, clinicians, and commissioners could all benefit from careful consideration of the evidence in this Collection for alternatives to surgery.
Author: Jemma Kwint, Senior Research Fellow, NIHR
How to cite this Collection: NIHR Evidence; Is surgery the best option? Research provides alternatives; November 2024; doi: 10.3310/nihrevidence_65060
Disclaimer: This publication is not a substitute for professional healthcare advice. It provides information about research which is funded or supported by the NIHR. Please note that views expressed are those of the author(s) and reviewer(s) at the time of publication. They do not necessarily reflect the views of the NHS, the NIHR or the Department of Health and Social Care.
NIHR Evidence is covered by the creative commons, CC-BY licence. Written content and infographics may be freely reproduced provided that suitable acknowledgement is made. Note, this licence excludes comments and images made by third parties, audiovisual content, and linked content on other websites.