A guide for the public on the latest physiotherapy research for the health and wellbeing of people with muscle, bone and joint pain
This was published in association with the Chartered Society of Physiotherapy, Keele University and Versus Arthritis.
All information in these materials are based on latest evidence and trusted clinical guidance. However, they were produced before the current global COVID-19 pandemic. We would therefore like to remind you to continue to adhere to guidance from the government and healthcare authorities when using or recommending these materials.
Introduction
Physiotherapy is important to help people manage pain in their muscles, bones and joints and to be as physically active as possible. There has been a large amount of research carried out into physiotherapy treatments over the past 10 years.
This is an easy-to-read guide which will tell you about some of the latest physiotherapy research relating to your problems with muscles, bones and joints (sometimes called musculoskeletal problems). This guide will give you information about treatment or exercise plans developed through research. You can use this information to discuss the treatment options available in your local area with a health care professional, such as your physiotherapist, doctor, nurse or pharmacist.
The guide has been developed for the public and patients, by patients and physiotherapists. It is intended for use by the public and can also be a quick reference guide for health care professionals. The work has been carried out by the National Institute for Health Research (NIHR), Keele University and the Chartered Society of Physiotherapy. It focuses on adults and covers seeking help from a physiotherapist for musculoskeletal problems through to treatment you may have at the hospital or community clinic. It also covers advice which will help you to manage your condition yourself at home. It does not cover broken bones and falls.
In my experience, research evidence is rarely or never shared with us patients. I think if it were then that might encourage us to take the exercises more seriously, if we could see the evidence of them being more effective.
Jennifer Bostock
How do I use this guide?
This guide gives you more information to help you make informed choices about getting help, understanding your treatment options and learning how to stay well in the longer term.
This has been created from a larger guide called Moving Forward – Physiotherapy for Musculoskeletal Health and Wellbeing. The larger detailed guide is aimed at physiotherapists but contains more information on the studies mentioned in this version. If you are interested in finding out more, you can read the full guide here.
What do I do if these treatments aren’t available in my area?
Physiotherapy services can vary from area to area but you do have the right to access treatment which is based on best available evidence. You can ask your GP, physiotherapist, nurse or pharmacist for more local information.
I’m thinking about how I can get treatment for my muscle, bone, or joint problem. What do I need to think about?
It may help you to think about the following questions:
“Do I know how and where I can access physiotherapy – from hospitals, community services, local GP surgeries, workplaces, community centres and leisure centres?”
“Can a physiotherapist explain how the treatment will help me to manage my pain and everyday activities, including work?”
“Can GPs and physiotherapists advise me on exercise videos and websites and refer me for exercise at leisure centres and community physical activity groups?”
“Do I know what to do at home and after physiotherapy, to help me to continue to improve and keep me as healthy as possible?”
“What do I need to do to motivate myself to seek help, seek treatment or advice, and stay well?”
Why is research important?
We need research to provide evidence that treatments work. It is equally important to show if some treatments are not effective in the way we thought they could be.
Research involves looking into a specific problem using a scientific method. This is done by turning the problem into a question and then doing the research to answer the question.

Research can help address common problems.
One in four people are affected by musculoskeletal conditions, which are the leading cause of pain and disability in the UK.

Research can help people back to work.
30.8 million working days were lost in 2016 due to musculoskeletal problems - the second leading cause of sickness absence at work.

Research can save the NHS money.
Caring for patients with musculoskeletal conditions is the third largest part of the NHS spend.
Seeking Help
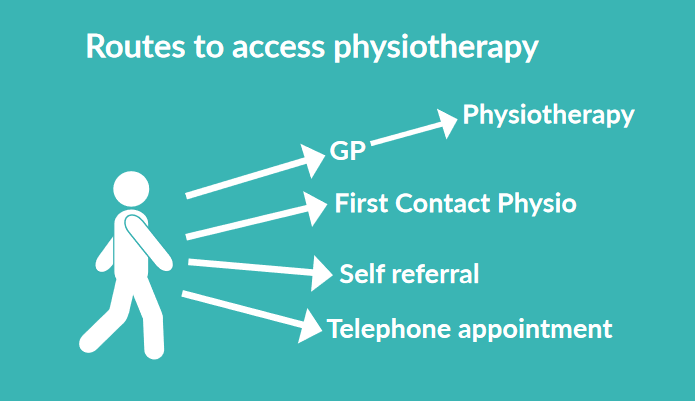
Routes to access physiotherapy:
- GP - physiotherapy
- First Contact Physio
- Self referral
- Telephone appointment
Research has shown us...
...that patients can access physiotherapy themselves directly
- Some areas of the UK allow patients to refer themselves directly to physiotherapy without having to go through their GP
- This is beneficial because it usually allows quick access to physiotherapy care
- Getting initial advice from a physiotherapist over the telephone (sometimes known as PhysioDirect) is safe and just as good as it is seeing them in person
- Face to face appointments can be made if necessary
...that physiotherapists can prescribe medication
- Some physiotherapists are trained to prescribe medicines
- Most patients are happy to have medication prescribed by their physiotherapist
- It is safe
...how to categorise people so that they can have the right care
- Every person is different – some people may need more support than others
- Questionnaires can help health care professionals and people to decide how much and what type of support they may or may not need
- This reduces investigations and treatments, disability and absence from work
What can I do when seeking help?
- Contact your GP surgery for a consultation with a First Contact Physiotherapist if your surgery has one
- Ask your GP surgery how you can directly access physiotherapy over the phone. This is sometimes known as PhysioDirect
- You can ask your pharmacist, physiotherapist, GP or nurse for more information about medications
- You can talk to your health care professional about the treatment that you both think is right for you
First Contact Physiotherapists – research underway
- First Contact Physiotherapists (FCP) have advanced skills and are able to care for people with a wide range of bone, joint and muscle conditions
- In areas where First Contact Physiotherapy is available, you can go directly to see a FCP at your GP surgery without needing to see a doctor
- The FCP can assess you and diagnose what’s happening, talk to you about medications and treatments, and give expert advice on how best to manage your condition
- They can refer you to specialist services if necessary
Jane's story
Jane has suffered with back pain for the last six weeks, which has become worse. This has stopped her from doing things she enjoys, such as her ballroom dance classes and has resulted in her being off work for the past week. Jane went to her GP practice to make an appointment with her doctor, and the receptionist advised that she could have an appointment directly with a First Contact Physiotherapist based at the practice. During her appointment, the physiotherapist discussed Jane’s symptoms and how her low back pain affected her, and they completed a short questionnaire together. The questionnaire helped the physiotherapist to give Jane the most appropriate treatment for her.
The physiotherapist gave her some initial advice about managing her pain, before referring her for group based talking therapies and exercise. After several sessions, Jane started to learn ways of coping with her back pain, pacing daily activities and continuing with her exercises, which helped to keep it at a manageable level. The physiotherapist also helped her to talk to her employer and get back to work. She now goes ballroom dancing once a week, which she loves.
For further information about the research studies which supported Jane to seek help, get treatment and stay well, go to the full review.
Getting Treatment and Staying Well

Treatment given by physiotherapists
- Exercise and activity
- Advice about your condition
- Medication advice
- Work advice
- Support for self management
Research has shown us...
... physiotherapists can help people at work
- Physiotherapists can spot issues that make it hard for people to return to work or keep fit for work
- They provide work related advice and support for people who find it hard to work with a muscle, bone and joint problem or return to work after having time off
- In some areas of the UK, physiotherapists provide advice over the phone and follow up with a face to face appointment if needed
- They can help people to have fewer days off work, perform better at work and give people improved confidence when returning to work
- This saves money for society by keeping people in work
... physiotherapists can help with exercise
- Exercise benefits people with osteoarthritis (a condition that causes joints to become painful and stiff) in their lower limbs, particularly knee osteoarthritis
- Physiotherapists provide exercise programmes that combine strengthening, flexibility and aerobic (strengthening the heart and lungs) exercise
- These types of exercise reduce pain and help people in their day to day lives
... physiotherapists can give you useful written advice
- Written advice for osteoarthritis is available in the form of an osteoarthritis guidebook
- Health care professionals receive training to be able to talk through the condition with the patient and also provide them with this written advice
- The training helps the health care professional to support the patient to learn to manage their condition themselves, for example through exercise and weight management. This improves the quality of care and advice received by patients
"Having being diagnosed with osteoarthritis in both knees I was given a booklet titled ‘A guide for people who have osteoarthritis.’ This booklet has been well researched by people from various organisations and sufferers of this painful and distressing condition. I found it to be very informative as it covered all aspects of osteoarthritis, offering not only sound advice on everyday living, but ways and means of coping with associated problems. Its use of simple language made it easy to read and the diagrams were a useful visual aid. All in all a helpful, practical and informative guide that all adults over the age of forty-five with osteoarthritis should have access to."
... group based exercise can work for knee pain
- Education and exercise groups can help people with long term knee pain, for example, the ESCAPE-Pain programme. Participants receive:
- Exercise plans
- Strategies for self-managing knee pain
- Myth busting
- Encouragement to keep doing regular activities after the programme
- Although this is group based, advice is tailored to each participant
- Classes can take place in leisure centres and physiotherapy departments and are value for money
- After completing the programme participants are able to move better and do more which improves their quality of life
- Participants take less pain relief and don’t need to see their GP as much
... classes plus exercising at home are important
- People who exercise at home as well as going to physiotherapist classes have greater improvement in walking, balance and lower limb strength compared to just completing home based exercise
... combined physical and emotional approaches are helpful for some people with low back pain
- Combining exercise with group talking therapy sessions for people who have had low back pain for six weeks or more improves quality of life
- This involves attending an initial assessment (up to 90 minutes) followed by six (90 minute) group sessions delivered by specially trained health care professionals
- These sessions include goal setting, pacing, challenging beliefs, managing pain and improving communication with health professionals
... physiotherapy can help with shoulder pain
- Most people receive treatment for shoulder pain from GPs or physiotherapists
- People who experience common causes of shoulder pain see greater improvements in pain and function with physiotherapist-led exercise compared with advice and exercise leaflets
... physiotherapy can support recovery from knee surgery
- Following a total knee replacement, physiotherapy is provided in hospital to help recovery before going home
- Physiotherapy is important for recovery to improve movement and strength, allowing people to gain the maximum benefit from surgery
- Physiotherapy after going home from hospital can improve day to day activity levels up to three months after knee replacement, but long-term benefits of physiotherapy are not known
... physiotherapy can also help people online
- There are resources online which support recovery after knee surgery. When a patient uses this tool and goes to face-to-face physiotherapy, their confidence and motivation increase
... acupuncture is not advised in low back and knee pain due to osteoarthritis
- Although acupuncture is not currently recommended in the UK for people with low back pain or in osteoarthritis, continued research will help inform future knowledge
... physiotherapists can promote good health
- Physical activity can help people to avoid developing other conditions
- A key role for a physiotherapist is to provide motivational support to help people to continue with exercises and activity outside of the clinic or hospital
"When I started the programme I couldn’t see how the pain in my limbs was going to go. My first goal was just to stand straight. Now I’m not hunched over and I’m beginning to walk properly. I’m still stiff, I’ve still got arthritis but what I don’t have is the pain. I’m not afraid to go out, I’m not afraid to cross the road....I feel better mentally as well as physically."
What can I do when accessing and getting treatment?
Work
- If work is a concern, talk to your physiotherapist or health care professional
Exercise
- Discuss exercise options which may be available to you
- Ask for written health information to support you to get better, for example https://startback.hfac.keele.ac.uk/patients/ or https://jigsaw-e.com/patient-focus/guidebook/
- Ask about group based exercise sessions for knee pain. These are sometimes called ESCAPE-Pain - https://escape-pain.org/living-with-joint-pain
- Think about asking whether a programme is available which offers both physical and emotional support.
- Talk to your physiotherapist about exercise as an alternative to surgery
Surgery
- If you have to have surgery, talk to your physiotherapist about exercise and access to physiotherapy to help you to recover. The availability of physiotherapy after discharge from hospital varies between local areas
Written Information
- Ask for written health information to support you to get better, for example an information leaflet, ap and animations form Keele University or this Osteoarthritis Guidebook
- Be cautious when using internet search engines about the quality of the information. Some online resources may not be accurate, if in doubt, seek advice from your health care professional
- See ‘further information’ at the end of this document for places you can find out more about research and physiotherapy
Abdulla's story
Abdulla’s knee has been troubling him for a few years. His knee pain is worse in the morning but by the time he’s up and showered it feels a bit better. Abdulla is an IT specialist and sits all day. He doesn’t feel confident exercising and also worries that moving may make his pain worse. His wife suggested he visits his medical practice and from there he booked an appointment with a First Contact Physiotherapist, who asked him some questions and looked at his knee, so that she could fully understand his problem.
Abdulla was told he had osteoarthritis. The First Contact Practitioner had completed specialist training on osteoarthritis and talked Abdulla through his condition, providing him with an information guidebook and told him about a local group based exercise class called ESCAPE-Pain. After this conversation, Abdulla realised that something had to change if he was going to feel better, so he decided to give it a try. Abdulla went along to the local community centre twice a week for six weeks and was given exercises that were tailored to him by a physiotherapist who works in the community. He learned that losing weight and moving more would help his pain, rather than making it worse, which is not what he had thought. He was also able to talk to other people in his situation who gave him some advice on how to fit exercise into his daily life. He has lost a bit of weight and is feeling more positive.
For further information about the research studies which supported Abdulla to seek help, get treatment and stay well, go to the full review.
Staying Well

Treatment given by physiotherapists
- Exercise and activity advice
- Advice about your condition
- Medication advice
- Work advice
- Support for self management
What can I do when trying to stay well?
- You may have ups and downs in the long term, but physiotherapists can help you over time – speak to them if you have any ongoing concerns
- Remember to stay as active as possible
Further Information
This guide has been created from a more detailed and comprehensive guide called Moving Forward – Physiotherapy for Musculoskeletal Health and Wellbeing. This larger guide is aimed at patients, local NHS organisations, physiotherapists and NHS commissioners, but contains more information on the studies mentioned in this Easy Read version.
Are you interested in being involved in research? If you would like to be involved in (but not participate in) research, go to People in Research. Being involved in Patient and Public Involvement and Engagement gives you the opportunity to use your experience of living with a musculoskeletal condition and advise researchers on how to keep their work patient focused and relevant. If you want to be a participant in research (i.e., receive the treatment that is being trialled in a research study) then you can visit Be Part of Research.
For accounts of real life patient and public involvement, visit Keele University School of Medicine’s Patient and Public Involvement and Engagement pages.
To learn more about how evidence from research is implemented into real world clinical healthcare, go to Keele's Impact Accelerator Unit.
To find out more about physiotherapy and physical activity, visit the Chartered Society of Physiotherapist’s Patient and Public pages.
NIHR Evidence is covered by the creative commons, CC-BY licence. Written content and infographics may be freely reproduced provided that suitable acknowledgement is made. Note, this licence excludes comments and images made by third parties, audiovisual content, and linked content on other websites.
