This is a plain English summary of an original research article. The views expressed are those of the author(s) and reviewer(s) at the time of publication.
Children with chest infections are often prescribed antibiotics. However, new research showed that they get little benefit from a commonly-used antibiotic (amoxicillin). The treatment did not offer value for money for the NHS.
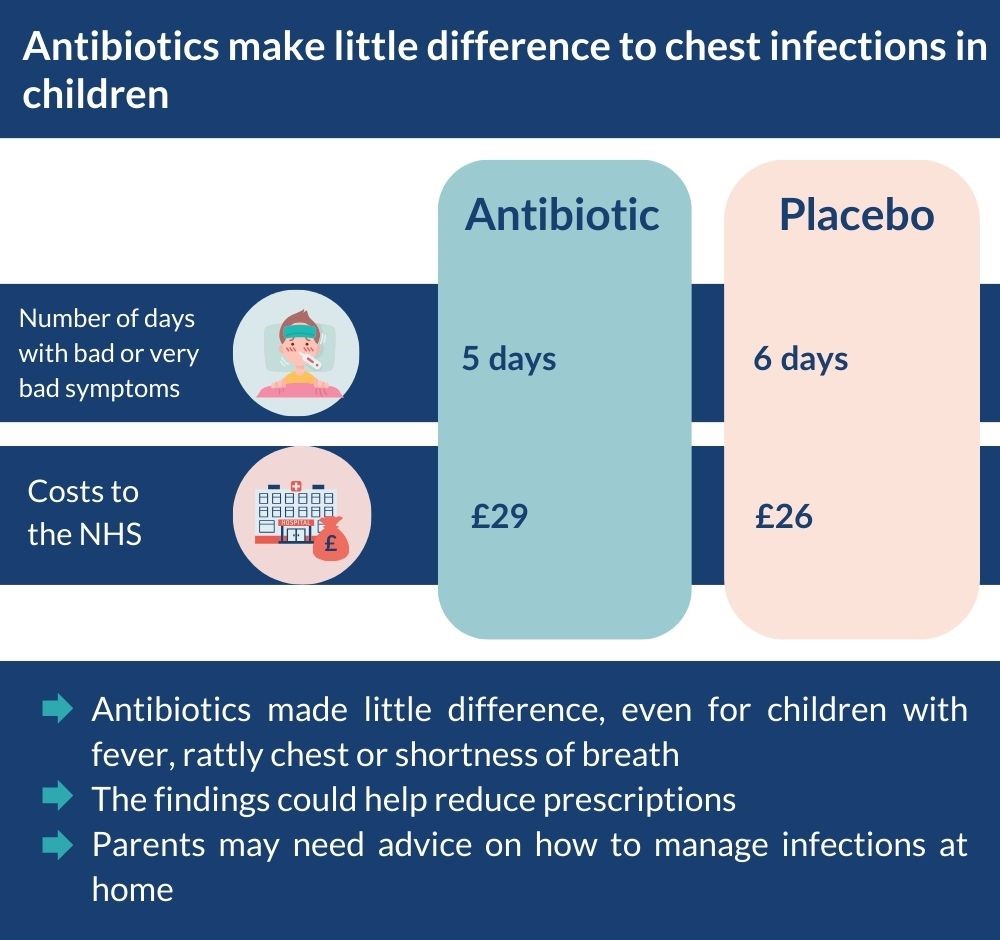
In a trial involving 432 children with a chest infection, half received the antibiotic and the others received a dummy drug (placebo). Children on antibiotics had bad (or worse) symptoms for 5 days, compared with 6 days for those on placebo. The findings were similar even for children with symptoms such as fever or shortness of breath.
For parents, this study provides reassurance that managing chest infections at home is safe, but they need advice about how and when to seek further medical help (if they suspect pneumonia, for example). The findings could help reduce antibiotic prescriptions and the spread of antibiotic resistance.
For more information on chest infections, visit the NHS website.
The issue: do children with chest infections need antibiotics?
Chest infections are one of the most common conditions seen in primary care. At least 2 in 5 children are prescribed antibiotics. But such infections are starting to become resistant to antibiotics, largely due to unnecessary prescribing in primary care. It is not clear whether antibiotics still work against many bacterial infections.
Parents want their child to recover quickly and many think antibiotics will help. However, there is limited evidence to support the use of antibiotics in primary care for children with chest infections.
Even when infections come with symptoms that more often prompt antibiotic use (fever, rattly chest, or some shortness of breath), there is little evidence to suggest that antibiotics are needed.
Researchers compared a common antibiotic (amoxicillin) with placebo in children with a chest infection in primary care. They also assessed the value for money of the antibiotic.
What’s new?
This randomised controlled trial included 432 children (6 months – 12 years) with a chest infection at 56 GP practices in the UK. They were excluded if pneumonia was suspected. Half (221) received antibiotics and half (211) received placebo for 7 days.
Families kept a diary for at least a week and recorded the number of days their child had symptoms (on a scale from no problem to as bad as it can be). The researchers also compared results in the group overall, with those children with additional symptoms that commonly trigger antibiotic use such as fever, a rattly chest, or shortness of breath.
Ahead of time, working with a patient and public involvement group, the researchers decided that antibiotics would be justified if they led to 3 fewer days with bad or worse symptoms.
The study found that:
- children on amoxicillin had bad or worse symptoms for 5 days, compared with 6 days for those on placebo (1 day less)
- the findings were similar even among children with symptoms or signs that more commonly trigger antibiotic use (such as fever or shortness of breath).
Side effects, the number of additional GP appointments, and hospital assessments/admissions for worsening symptoms were similar between treatment groups.
Throat swabs confirmed whether bacteria were present. Antibiotics were not significantly more effective in children with a confirmed bacterial infection (4 days of bad or worse symptoms) than in those without (6 days).
The costs to the NHS per child were similar for those receiving amoxicillin (£29) and placebo (£26). The wider costs to society (including time off work) were the same, £33 each.
The researchers interviewed 16 parents and 14 clinicians about their experience of managing chest infections. Parents found it difficult to gauge their child’s symptoms, and often judged severity by the sound of the cough. Parents accepted that antibiotics should only be used when necessary. Clinicians noted parents are more accepting of not being prescribed antibiotics than in the past, with many being satisfied with an assessment, reassurance, and advice.

Why is this important?
The study found that amoxicillin is unlikely to be effective or cost-effective for children with chest infections. Interviews showed that parents found it difficult to assess symptom severity. Parents could benefit from advice from GPs on how to manage infections at home, as well as how and when to seek medical help if they are concerned.
The findings will encourage GPs not to prescribe antibiotics for children with chest infections, even those with fever or other symptoms that commonly trigger a prescription. Reductions in antibiotic use could slow the spread of antibiotic resistance.
The trial was interrupted by the pandemic, and did not include the initial planned number of children. However, the numbers were sufficient to be sure that most groups of children who received antibiotics did not benefit meaningfully. If there were smaller differences (less than 3 days) between different groups of children (according to their symptoms), these might not have been picked up. Only amoxicillin was tested; other antibiotics may be more effective.
What’s next?
The researchers are developing a tool for clinicians to assess a child’s risk of worsening illness and make suggestions about how to treat them. This could help target antibiotics for those who would benefit most. But the tool still needs to be thoroughly tested.
You may be interested to read
This is a summary of: Little P, and others. Antibiotics for lower respiratory tract infection in children presenting in primary care: ARTIC-PC RCT. Health Technology Assessment 2023; 27: 1 – 120.
The trial was reported in: Little P and others. Amoxicillin for acute lower respiratory tract infection where pneumonia is not suspected clinically: a 12 country randomised placebo controlled trial in primary care. Lancet Infectious Disease 2013; 13: 123 – 9.
Information on chest infections from NHS Inform.
Another study showing limited benefit of antibiotics for chest infection: Butler C, and others. Variation in antibiotic prescribing and its impact on recovery in patients with acute cough in primary care: prospective study in 13 countries. British Medical Journal 2009; 338: 1 – 8.
Funding: This study was funded by the NIHR Health and Technology Assessment programme.
Conflicts of Interest: Some authors have received fees and funding from pharmaceutical companies. Details are available in the original paper.
Disclaimer: Summaries on NIHR Evidence are not a substitute for professional medical advice. They provide information about research which is funded or supported by the NIHR. Please note that the views expressed are those of the author(s) and reviewer(s) at the time of publication. They do not necessarily reflect the views of the NHS, the NIHR or the Department of Health and Social Care.
NIHR Evidence is covered by the creative commons, CC-BY licence. Written content and infographics may be freely reproduced provided that suitable acknowledgement is made. Note, this licence excludes comments and images made by third parties, audiovisual content, and linked content on other websites.