A dynamic review of the evidence around ongoing Covid19 (often called Long Covid). You can also download this review as a PDF.
- Executive summary
- NIHR Centre for Engagement and Dissemination
- What are we aiming to achieve with our Living with Covid19 reviews?
- Framing the evidence
- What is ‘Long Covid’?
- How many people who have had Covid 19 will experience ongoing symptoms?
- The causes of Long Covid
- Impact of Long Covid on daily living
- Diagnosing and predicting the course of Long Covid
- Management of Long Covid
- Conclusion
Executive summary
This is the second of two dynamic reviews of the evidence around people’s experience of the enduring symptoms following a Covid19 infection.
We published our first review of the evidence in October 2020. At the time there was uncertainty about the extent to which there could be lasting effects, and most people assumed a linear progression of a severe acute infection with a long recovery tail. Our first review on “Living with Covid19” was informed by the experience of professionals and we worked closely with a group of people with lived experience. In this review, we focus on the published evidence. In addition, we report findings from a short survey of people living with Covid19 that we embedded on our website. With over 3,000 responses it provided us with an insight into the key issues and challenges for people living with Covid19.
Since October, the term ‘Long Covid’ has gained widespread use and we have adopted it. But we recognise it covers a wide range of symptoms, including a high number of post-viral fatigue cases that appear to resolve spontaneously by 8 to 12 weeks.
There is enormous variation in the estimated prevalence of Long Covid due to different measurement criteria, making comparing studies impossible. Many people were unable to access Covid19 testing when first ill and are excluded from some studies as the infection is not confirmed. This may mask the true prevalence of Long Covid. Uncertainty about a prior infection means some people report difficulty accessing services for their Long Covid symptoms. It appears that at least 10% of those infected with Covid19 experience at least one symptom for 12 weeks or longer. For those who were not admitted to hospital, at least 20-30% experience at least one enduring symptom around one month later and at least 10% three months later. For those who were admitted to hospital, between 50% and 89% have at least one enduring symptom after two months. Our own and Davis et al. (2020) preprint surveys suggest significant rates of Long Covid beyond six months for people who were not hospitalised. Any estimates of incidence and prevalence must be considered provisional. The ONS reported an incidence in December 2020 of 301,000 people in the UK with symptoms lasting between 5 and 12 weeks. Long Covid appears to be more frequent in women and in young people (including children) than might have been expected from acute Covid19 mortality.
Whilst there is a growing list of symptoms associated with Long Covid, we know little about different clusters and patterns of symptoms (sometimes described as phenotypes, syndromes or clusters). There is increasing evidence of organ impairment in both people who were admitted to hospital and those who stayed at home. The limited evidence of correlation between past history and current pathology would suggest a need to investigate anyone with persistent symptoms, including those who were never admitted to hospital.
There is also evidence of a group of people with cognitive processing disorders and anxiety with some indication of neurological rather than social cause. A substantial number of people have symptoms they are not yet understood. Some are similar to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and others to orthostatic intolerance syndromes. There is some evidence suggesting Long Covid is a still active disease, with immunological evidence of continued inflammatory responses, lingering viral activity and/or blood clotting disorders. For some people with Long Covid, there appears to be the potential for further deterioration.
Long Covid can be very debilitating and some people need help with personal care months after the initial infection. 71% of respondents in our own survey said Long Covid was affecting family life and 39% said it was impacting their ability to care for dependents. This is having an impact on the workforce, with 80% of respondents in our own survey saying Long Covid had affected their ability to work and 36% said it was affecting their finance.
Long Covid can be a multi-system disease, and some people may have active disease that needs ongoing monitoring in secondary care. This will require joined-up care management across specialities and between primary and secondary care. New service delivery models that provide rapid access to an increasing number of people with Long Covid need to be designed and evaluated. This will also require a multiprofessional workforce strategy.
As well as clinical rehabilitation care, some people need ongoing social care. Particular attention should be paid to the impact of Long Covid on vulnerable people, (such as older people with pre-existing health conditions) who may not have been captured in research to date and who may be tipped into a state of frailty.
We conclude that the journey of Long Covid is not well understood and it is important to continue to listen to the lived experience as we move into the second year of this new disease. As we learn more about the progression of Long Covid, it is important to retain a wide range of working hypotheses.
We make the following recommendations for the future research agenda.
- More research is needed on the incidence of Long Covid and its causes. This will help to predict and prevent Long Covid in the longer term. There is an urgent need to research treatments and management for people with Long Covid.
- The emergent nature of the understanding of Long Covid emphasises the need to continue to explore a range of hypotheses in any research that is undertaken.
- A precursor to research in all areas is a better understanding of the disease syndromes and symptom clusters that currently sit under the umbrella of Long Covid or post Covid.
- We recommend that a minimum data set for recording a wide range of symptoms be agreed and used by both researchers and healthcare providers.
- Some elements of Long Covid are similar to other conditions and evaluations of interventions (pharmaceutical, psychological and physical therapies) that may improve symptoms. We recommend evaluation of the use of interventions that have been effective in other conditions when used with people with Long Covid. For non-pharmaceutical interventions, a range of research methodologies should be encouraged.
- Long Covid is a significant health burden that is unlikely to be met by existing NHS services and new delivery models that allow rapid access are needed. We recommend rapid evaluation of different service models and skill mix for supporting people with Long Covid.
- Seldom heard voices are not visible in the current evidence. We recommend research that is targeted at vulnerable people (including older people and people with learning disabilities) as well as hard-to-reach groups including travellers and prison populations.
- We recommend that people living with Long Covid (who are experts by experience) should be equal partners in setting the research agenda.
NIHR Centre for Engagement and Dissemination
The NIHR aims to engage people in knowledge exchange to develop and improve health and social care. One of the ways we do this is through our Themed Reviews. These are not systematic reviews of all the evidence nor are they guidance or recommendations for practice. Instead they are narratives based on a selection of different kinds of evidence chosen to illuminate and inform discussions focused on actions for practice. As far as possible, they highlight UK evidence that takes into account the UK infrastructure and culture, often funded by the NIHR. Themed reviews include both academic study and practical wisdom from lived experience and are guided by our stakeholders.
What are we aiming to achieve with our Living with Covid19 reviews?
Our first review on “Living with Covid 19” was informed by the lived experience of patients and professionals and we worked closely with a group of people with lived experience. In this review, we turn our attention to the published evidence. In addition, we report findings from a short survey for people living with Covid19 that we embedded on our website. As with many surveys, it was a self-selected sample that may not be representative of all people living with enduring symptoms. But, with 3,286 full responses it provides valuable insight into key issues and challenges for people living with Covid 19. This review may be particularly helpful for professionals who are increasingly coming into contact with people with Long Covid, but not running specialist services themselves. It may also be helpful for the families or employers of people experiencing Long Covid as well as people living with enduring symptoms.
Since October, there has been widespread acceptance that long-term symptoms exist and there is increasing activity to refine measurement. NHS England and the Scottish Government asked the National Institute for Health and Care Excellence (NICE) and the Scottish Intercollegiate Guidelines Network (SIGN) to develop guidelines on the long-term effects of Covid19. Working with the Royal College of General Practitioners, the first of their ‘living’ guidelines was published on 18th December 2020. In November 2020, the NIHR, together with United Kingdom Research and Innovation (UKRI) issued a call for research into the longer-term effects of Covid19 in non-hospitalised individuals. Successful bids were announced on 18th February 2021.
Framing the evidence
More papers have been published since our last review, but the evidence still resembles a ‘Swiss cheese’ with many gaps. Inconsistencies in findings reflect different assumptions in the research design. In this review, we try to make sense of the disparate body of literature and clarify what is known, what needs further research, and most importantly, what we know about treating Long Covid.
This report is not a systematic review of all published evidence. We have not formally assessed the quality of the included evidence. We searched academic databases and sought recommendations from a network of people looking at Long Covid. We identified 302 publications, some of which were opinion pieces or personal stories. We narrowed this down to research papers that addressed three themes: how common is Long Covid? What causes Long Covid? and how might Long Covid be treated? The team decided which papers to include in this review based on how they added to the narrative. We intend to outline a coherent picture from some of the jigsaw pieces of evidence, and we make no claims of completeness.
In our first review, we opted to exclude preprints because they had not yet been peer-reviewed. We still read them with caution, however they identify themes that are relevant to policy, practice and future research questions, so we discuss their findings as propositions rather than as assured evidence. Where we reference them, we identify that they are preprints. The nature of research reporting means that many papers describe data collected at an early stage of the pandemic and therefore cannot include detailed information about the current duration of symptoms. This also means that we do not know the impact of new variants or vaccinations on rates of Long Covid (however defined). Whilst we do not think the evidence can be synthesised, it can be used to build a three dimensional picture of Long Covid and to illuminate what further questions need to be asked. Summaries of included studies can be found in Appendix A.
What is ‘Long Covid’?
One of the features of Long Covid is the wide range of symptoms. Davis et al. (2020) preprint lists 205 different symptoms related to 10 different systems. For some people, it has a relapsing nature, often referred to as the ‘corona coaster’, and for others, there is a single symptom but with atypical progress. This has significant implications for the management of the disease.
More than one syndrome
Our first review was mindfully called ‘Living with Covid19’ to capture a range of symptoms that persist following a Covid19 infection. We noted that people may experience different clusters of symptoms or syndromes (see Figure 1). We proposed that some people suffered permanent organ damage and there may also be a number of distinct syndromes, including post intensive care syndrome, post viral fatigue syndrome and long-term Covid syndrome. We also observed that some people may be suffering with more than one syndrome at the same time.
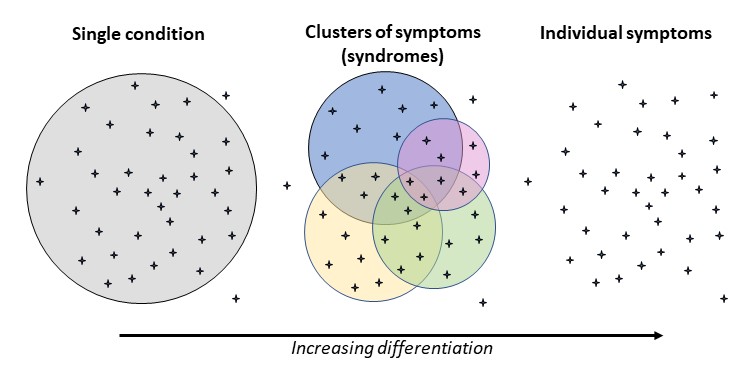
Figure 1: Measurement of symptoms, clusters or individual conditions. Please click here for a text description of this figure.
Since then, others have been reaching similar conclusions about distinct patterns. Ayoubkhani et al. (2021) preprint reporting on the Office for National Statistics (ONS) work notes that Long Covid, or post-Covid syndrome, is not a single condition and Yong's (2020) preprint noted multiple different symptoms and potential disease mechanisms and recommend that future research should consider subtypes of Long Covid. Cirulli et al. (2020) preprint report of a large cohort study in the USA describes diverse phenotypic presentations. Some authors have attempted to classify the different syndromes.
Venturelli et al. (2021) followed up patients discharged from hospital in Italy and noted three different syndromes “it appears reasonable to try and separate those symptoms related to post-viral chronic fatigue syndrome, from those due to post-critical-illness syndrome, or post-traumatic stress disorder”.
Sudre et al. (2020) preprint reported two different patterns of symptomatology for Long Covid from the Zoe Covid Symptoms Study App; firstly, people reporting exclusively fatigue, headache and upper respiratory complaints (shortness of breath, sore throat, persistent cough and loss of smell) and secondly those with additional multi-system complaints, including ongoing fever and gastroenterological symptoms. Amenta et al. (2020) propose three classifications: 1) residual symptoms that persist after recovery from acute infection; (2) organ dysfunction that persists after initial recovery; and (3) new symptoms or syndromes that develop after initial asymptomatic or mild infection. The Cochrane Rehabilitation 2020 rapid living systematic review (Ceravolo et al. 2020) used four categories that might relate to Long Covid: 1) symptoms continuing from the acute phase of Covid19 and its treatment; 2) symptoms causing a new health condition; 3) late onset symptoms appearing as a consequence of Covid19 but after the end of the acute phase; 4) impact on a pre-existing health condition or disability.
Undulating symptoms and relapses
Salmon-Ceron et al. (2020) found that 43% of people followed up after discharge from a Paris hospital had a symptom-free interval before relapsing. They also report that 76% presented new symptoms that were absent during the acute phase of their Covid19 infection. Davis et al (2020) preprint paper of an international web-based survey, led by people with Long Covid, reported 86% of respondents experienced relapses occurring in an irregular pattern, or in response to specific triggers (such as physical or mental activity, stress, menstruation, heat, or alcohol). Our survey findings confirm the undulating nature of Long Covid symptoms described in our first review with 64% of respondents reporting a period of wellness before relapsing.
Use of time frames to segment the patient population
Some have categorised ongoing symptoms by duration, noting significant resolution rates at 5 weeks and again at 12 weeks. The NICE guideline published in December 2020, together with SNOMED codes for medical records released in the same month, divide symptoms into three time periods; acute Covid19 up to 4 weeks; ongoing symptomatic Covid19 from four to 12 weeks; and post-Covid19 syndrome developing during or after an infection consistent with Covid19 and continuing for more than 12 weeks and not explained by an alternative diagnosis. The NICE categories do not relate to particular symptoms or groups of symptoms.
Lived experience perspectives
Callard and Perego (2020) described how patient advocates rather than researchers created the narrative and the name Long Covid after connecting on social media and making visible the persistent nature of a wide range of symptoms when attention was primarily focused on acute illness and mortality. They noted that the ‘biphasic’ disease pathway description of ‘acute illness’ and ‘post-acute illness’ did not match the lived experience reports of multiple and diverse ongoing symptoms. Some patient advocates are unhappy with the term ‘post Covid’ as it suggests there is no active disease process. They point to both the evidence on continuing viral presence and the presentation of new symptoms after 12 weeks (see section on what causes Long Covid). NICE’s rationale for describing ‘post’ Covid19 syndrome was that it reflected that the acute phase of illness had ended and they did not intend for it to indicate that the person had recovered.
Key points
Researchers have categorised ongoing symptoms following a Covid19 infection both by their duration and by the number of symptoms. The difference in their findings raises a question about whether different people need different treatment and support. Indeed the duration of symptoms may correlate with different syndromes or phenotypes and may be related to different causal mechanisms.
How many people who have had Covid 19 will experience ongoing symptoms?
Why is this important?
Understanding how many people experience Long Covid is important for a number of reasons. Firstly, the need to plan adequate services (including assessment, diagnosis, treatment and supportive care) and the workforce to deliver them. Secondly, knowing how many people have ongoing problems informs decisions about funding for further research. Thirdly it helps to calculate the potential impact on society in the future, including the impact on those of working age and by extension the economy. Finally there may be a new generation of carers for those with Long Covid who have their own needs.
Methodological challenges
The lack of a consistent definition of Long Covid makes assimilating findings from different studies difficult. As Figure 2 demonstrates, studies have focused on different people, symptoms and time intervals, and used different sample sizes. The early lack of awareness of the range of symptoms associated with Covid19 meant that many people did not associated their symptoms with Covid19 and therefore did not associate their enduring symptoms with Long Covid. Conversely, the range of Long Covid symptoms is not widely known and people may not associate them with a prior Covid19 infection.
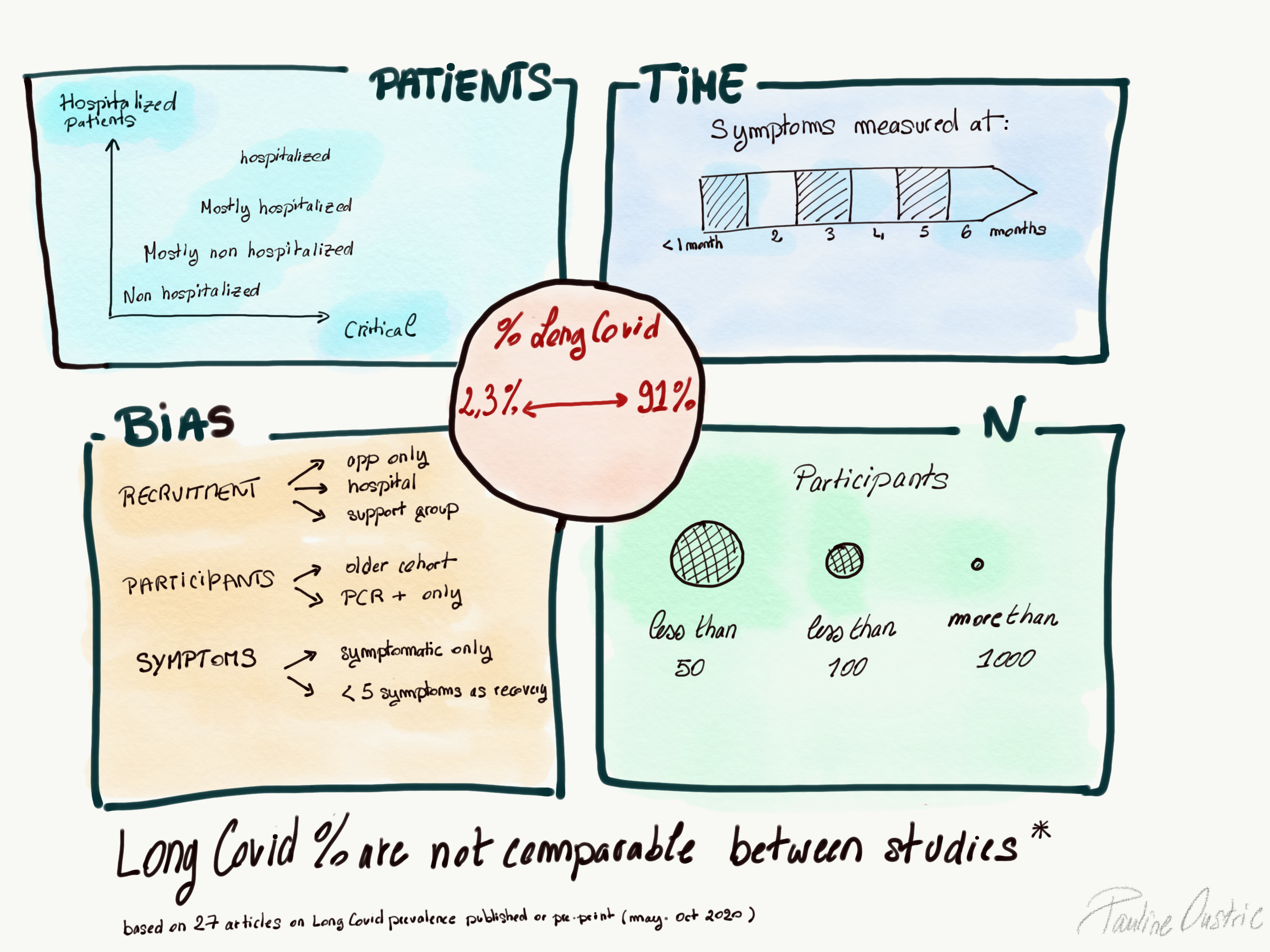
Figure 2: A diagram exemplifying that Long Covid prevelances are not comparable between studies. Please click here for a text description of this figure.
For many studies, a positive antigen, polymerase chain reaction (PCR), or antibody test is required to exclude people with symptoms not associated with a Covid19 infection. However, in the UK community testing was suspended in the UK in March 2020 and 82% of respondents to our survey said community testing was not available at the time of their initial infection. This lack of testing was also noted by Varsavsky et al. (2021), who reported that only 40% of those who reported classic symptoms on the Zoe Covid Symptom Study App had gone on to receive a test. In our survey, 56% of respondents had either had an antigen test or an antibody test at a later date. Of those tested, 46% tested negative, despite having had symptoms consistent with the virus. 67% of respondents were told by a health professional that their symptoms might be due to Long Covid. Barker Davies (personal communication), reporting on the UK Defence Medical Rehabilitation Centre video assessment service, found that service personnel who had not been admitted to hospital were 75% less likely to have had a test confirmation than those who were admitted to hospital. They also found that those had received a test confirmation of Covid19 had their assessment earlier than those who without a confirmation (8.5 weeks v 16 weeks). The inability of a significant number of people reporting Long Covid symptoms to confirm an initial infection means sampling in some of the studies may have been skewed.
Most studies report the frequency of at least one symptom, not necessarily the same symptom, rather than a cluster of symptoms. Many of the symptoms reported occur in a range of diagnoses, and a few studies have used controls to see if enduring symptoms are more common after a Covid19 infection. For example, Cirulli et al. (2020) preprint of a large public health study in the USA showed that whilst people both with and without a history Covid19 reported persistent new symptoms over three months, those who tested positive for a Covid19 reported them twice as often.
Box 1: Primary research studies (N.B. different research questions and designs means size of sample is not necessarily an indicator of relative quality)
| Study | No of participants in study |
| Ayoubkani et al. (ONS) | 47,780 Covid19+ hospital discharges (matched to controls) |
| ONS January 2021 update | 9,063 Covid19+ with LC symptoms (from CIS survey of 150,000) |
| Sudre et al. (Zoe App) | 4,182 |
| Davis et al. | 3,762 |
| NIHR survey | 3,286 |
| Munblit et al. | 2,649 |
| Vaes et al. | 1,837 |
| Huang et al. | 1733 |
| Venturelli et al. | 767 |
| Ciculli et al. | 357 Covid19+ ( 24,592 non-matched controls) |
| Xiong et al. | 538 |
| Mandal et al. | 384 |
| Hampshire et al. | 361 Covid+ (83,924 non-matched controls) |
| Tenforde et al. | 292 |
| Moreno-Perez et al. | 277 |
| Bergamaschi et al. | 207 |
| Dennis et al. | 201 |
| Logue et al. | 177 |
| Barker Davis et al. | 155 |
| Carfi et al. | 143 |
| Landi et al. | 131 |
| Buonsenso et al. | 129 |
| Townsend et al. | 128 |
| D’Cruz et al. | 119 |
| Arnold et al. | 110 |
| Tomasoni et al. | 105 |
| Halpin et al. | 100 |
| Puntmann et al. | 100 |
| Tabacof et al. | 84 |
| Salmon-Ceron et al. | 70 |
| Raman et al. | 58 |
| Vlachou et al. | 39 |
| Guedj et al. | 35 |
| Doykov et al. | 20 |
| Yeoh et al. | 27 |
| Humphreys et al. | 18 |
| Kommoss et al. | 13 |
| Dani et al. | 6 |
| Ludvigsson et al. | 5 |
Range of prevalence estimates
Measurement is reported as either prevalence (proportion of a known population at a specified point in time) or incidence (rate of new cases within a defined period of time). The prevalence estimates within the UK and internationally (see Figure 3) vary widely, even when measuring the same time frame. Estimates of people with symptoms that have not resolved by eight weeks range from 4.5% of people completing the Zoe Covid Symptom App (Sudre et al. 2020 preprint) to 89% of people who received a minimum of oxygen therapy in hospital for more than 48 hours (D’Cruz et al. 2020). However, the studies used different case definition and different inclusion criteria and therefore cannot be directly compared. The NICE guideline (2020) evidence reviews 2 and 3 noted the range of symptoms reported across studies was very broad and that all the studies reviewed were at high or moderate risk of bias.
Seldom heard groups such as travellers, prison populations, frail elderly people, care home residents, those with learning disabilities and children are not well represented in the data. Published studies may therefore not be representative of everybody who has Long Covid.
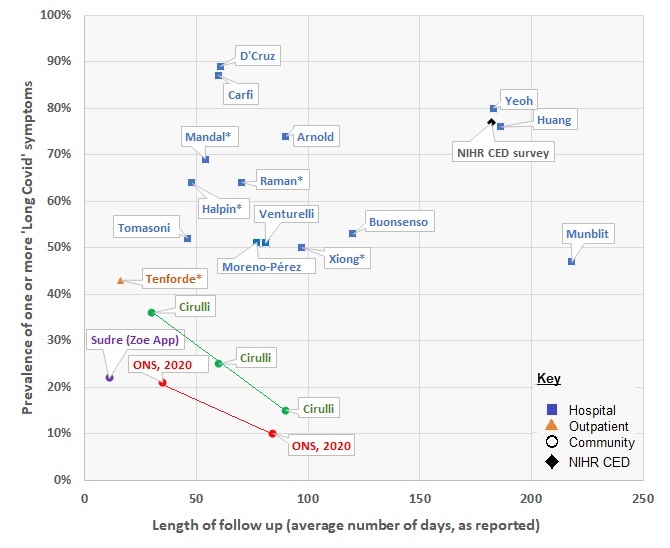
Figure 3: Range of prevalence estimates by duration. Please click here for a text description of this figure.
Studies also differ in the way they collect data. Some follow up a cohort of people (a fixed group of people studied over time), others use cross-sectional surveys (a sample of people studied at a point in time, and these differ between samples chosen to represent everyone in the population and those where people self-select).
Estimates of the proportion of people who experience Long Covid post-hospital discharge are more robust than for people who were not hospitalised. Studies published to date show that a higher proportion people who had been admitted to hospital go on to experience Long Covid, although this may reflect definitions of Long Covid that relate to a particular set of symptoms more common in those who were hospitalised (see section on what is Long Covid). We also note that criteria for being admitted to hospital vary across countries. Even in the UK, reports do not always differentiate between the different levels of care (those who received standard oxygen therapy, high flow oxygen or Continuous Positive Airway Pressure therapy [CPAP] and those who were mechanically ventilated).
Symptom reporting up to 4 weeks
Early studies looked at short term effects. For example, Tenforde et al. (2020) conducted a multistate telephone survey in the USA of 292 adults who had a positive test result for Covid19 but were not admitted to hospital, finding 35% had not returned to their usual state of health 2 to 3 weeks after testing. This included 20% of 18–34 years with no pre-existing conditions.
Symptom reporting from 5 to 12 weeks
The ONS (January 2021) estimated that 20% of all people in the UK who had tested positive for Covid19 exhibit symptoms for 5 weeks or longer and 10% exhibit symptoms for 12 weeks or longer. They reported an incidence of 301,000 people with symptoms lasting between 5 and 12 weeks for the week commencing 27th December 2020.
These are provisional estimates that may be revised as the follow-up data mature and the study methodology is developed. The ONS survey collects data from a random, representative sample of the community population in the UK through the Coronavirus Infection Survey (CIS). Everyone in the sample is swabbed at every follow-up visit, irrespective of symptoms or recent contacts. Thus there is no dependence on the broader community testing paradigm of the day. ONS have added a new question to the CIS survey in 2021 allowing respondents to state the impact Long Covid has had on their day-to-day activities, and including an expanded list of symptoms. Recognising that some people with symptoms may test negative this question will not be dependent on a positive test finding.
People admitted to hospital have been followed-up more often than those who stayed at home. D’Cruz et al. (2020) followed up people eight weeks after discharge from a UK hospital and found only 11% had no lasting symptoms; 39% were more breathless and/or had a persistent cough; 57% reported sleep disturbance; and 25% demonstrated post-traumatic stress disorder. Halpin et al. (2021) followed up people from another UK hospital on average six weeks after discharge and reported that 72% of post ICU patients and 60% of those treated on the wards reported new illness-related fatigue. Both groups reported breathlessness and psychological distress. 69% of ICU patients and 46% of ward patients reported lower health-related quality of life scores. These UK studies mirror international findings. Xiong et al. (2020) reported that 50% of patients discharged from a hospital in Wuhan reported one or more persistent symptoms three month later. Carfì et al. (2020) found that 87% of patients discharged from a Rome hospital after a Covid19 infection were still experiencing at least one symptom two months after the onset on Covid19 and 40% said that the quality of their life had been reduced. Tomasoni et al. (2021) found that 52% of patients discharged in Milan reported persistent physical symptoms between one and three months after they had recovered from a Covid19 infection and 17% reported persistent cognitive disorders. Mini–Mental State examination of 25 of the patients demonstrated scores that were compatible with cognitive impairment in 40%.
Moreno-Perez et al. (2021) prospective cohort study of adult patients in Spain presenting at an emergency department with varying severity of disease reported that 50% had a post-acute Covid19 syndrome (Long Covid) ten to 14 weeks after the infection. Cirulli et al. (2020) preprint paper reports an online survey of 21,359 people self-selected from existing cohort health studies in the USA to control for Covid19. Respondents were categorised into three groups for comparison; those who tested positive for Covid19, those who tested negative for Covid19 and those not tested at all. All were asked about new symptoms (due to any illness) that had lasted longer than 30 days. 15% of those who had tested positive for Covid19 were still experiencing symptoms lasting three months or more, compared to 8% of those who had never been tested.
The lowest estimate of enduring symptoms came from Sudre et al. (2020) in their October preprint reporting on 4,182 self-selected people who entered data on the Zoe Covid Symptom Study App and had tested positive for Covid19. They found 4.5% reported having symptoms lasting more than eight weeks and 2.3% having symptoms for longer than 12 weeks.
Symptom reporting at six months
Huang et al. (2021) reported on the follow up of patients discharged from a hospital in Wuhan following a diagnosis of Covid19. 76% of patients reported at least one symptom 6 months after the infection onset, with incidence higher in women. Logue et al. (2021) surveyed people with confirmed Covid19 infection in the USA, 85% of whom had not been hospitalised. 33% of non-hospitalised and 31% of hospitalised patients reported at least one persistent symptom six months after diagnosis. Munblit et al. (2021) preprint follow-up of patients discharged from a Russian hospital found that 47% reported one persistent symptom six to eight months later and 11% had multi-system symptoms.
Demographics
The profile of people with Long Covid does not seem to match those hospitalised with Covid19 or those who die from it. Most surveys indicate that Long Covid is more commonly reported by women (Yong, 2020; ONS 2020; Sudre et al. 2020 Davis et al. 2020; Munblit et al. 2021) including our own, where 81% of respondents were female, and we discuss possible biological sex differences in the section on what causes Long Covid. However, most research findings do not then report in detail whether the experience of Long Covid differs by sex. There is little discussion about ethnicity in Long Covid, although this may be a sampling issue. Cirulli et al. (2020) preprint reports an investigation using a pre-existing public health cohort study in the USA that matched people who reported a Covid19 infection with controls (people already in the cohort study but who had not had a Covid19 infection). They found no differences between ethnicities in overall rates of long-term symptoms, although they acknowledged that the sample size of non-white ethnicities was limited.
Long Covid appears to be more common in younger people than would be anticipated from the rates of hospitalisation for Covid 19. 67% of respondents to our own survey were aged between 25 and 54 and Davis et al (2020) preprint report 87% of people responding were aged 30-59.
There is growing evidence of Long Covid in children. Buonsenso et al. (2021) preprint followed up children who presented to an Italian hospital with Covid19, excluding those with severe disabilities. 53% had at least one persisting symptom four months after diagnosis and 43% reported that it affected their daily activities. They note that three children developed multisystem inflammatory syndrome; this syndrome in children with Covid19 is also noted by Ahmed et al. (2020) systematic review. Ludvigsson et al. (2020) case report described five children with symptoms lasting for six to eight months after a clinical diagnosis of Covid19. None were hospitalised and although improving, none had returned to school. The Office for National Statistics (ONS), in their January 2021 update based on their CIS household survey, estimated that 12.9% of 2-11 year olds and 14.5% of 12-16 year olds in the UK were still experiencing one of the symptoms in the survey five weeks after testing positive for Covid19.
Key points
Prevalence estimates cluster into broad groupings, although caveats around bias and representation mean they should be treated with caution. For those who were not admitted to hospital, it appears that at least 20-30% experience at least one enduring symptom around one month later and at least 10% three months later. For those who were admitted to hospital, between 50% and 89% have at least one enduring symptom after two months and more recent studies suggest there is still a high prevalence at six months. Our own and Davis et al. (2020) preprint surveys suggest significant rates of Long Covid beyond six months for people who were not hospitalised. Any estimates of incidence and prevalence must be considered provisional. Long Covid appears to be more frequent in women and in young people (including children) than might have been expected from acute Covid19 mortality. There is little data about ethnicity and the incidence of Long Covid in these groups is unclear.
The causes of Long Covid
This section looks at the evidence about what causes Long Covid and its impact physically, psychologically and socially. Understanding the cause of Long Covid would help design treatments and to prevent it. Much of the evidence is speculative, based on the symptoms people with Long Covid display or generalising from conditions with similar symptoms. It is unclear whether the same pathology seen in the acute phase of Covid19 also leads to Long Covid. As Yong’s (2020) preprint observes, one puzzling feature of Long Covid is that its development is not predicted by initial Covid 19 severity.
We do not know whether symptom patterns reflect already known syndromes or a unique new disease of Long Covid. Salmon-Ceron et al. (2020) raised several theories about the cause of Long Covid: continuing presence of the virus, reinfection (the same or possibly a different strain), dysfunctional immune response leading to an inflammatory chronic condition, or a condition similar to ME/CFS. They observed that post-traumatic stress could not be dismissed as a factor.
Post Viral Fatigue
The most commonly reported enduring symptom following the onset or Covid19 is fatigue. This is a well-established symptom following viral infections and was noted after the Spanish Flu pandemic and the more recent SARS, MERS and Ebola epidemics. Fatigue is also observed after some bacterial infections. Lam et al. (2009) report a follow-up study of 233 patients with Severe Acute Respiratory Syndrome (SARS) in Hong Kong which showed that 40% met the criteria for Chronic Fatigue Syndrome at four months and 27% for longer than six months.
Immunology
The fact that so many physiological systems are involved in Long Covid led the British Society for Immunology (2020) to suggest that damage caused by the immune system’s response, rather than the virus itself, may be causing the symptoms. Barker Davies et al. (2020) noted inflammatory changes seen in Covid19 can result in inflammation of blood vessels, myocarditis (inflammation of the heart muscle) and arrhythmias (heart beat irregularities) which may explain some of the symptoms and diagnostic findings in Long Covid. This is borne out in Raman et al. (2020) paper that found damage visible on MRI scans beyond just the lungs and reduced exercise tolerance correlated with serum markers of inflammation.
The British Society for Immunology suggest that inflammatory responses may worsen pre-existing conditions, but equally may cause new ones. They also note that inflammation can lead to thrombotic complications. Bergamaschi et al. (2020) preprint demonstrated that people needing hospital admission had delayed immune responses and conclude that late inflammatory changes and persistent cell defects may contribute to Long Covid. Doykov et al. (2020) analysed blood samples from healthcare workers who had tested positive for Covid19 who were asymptomatic or who had a mild acute infection and compared their mass-spectrometry-based assay profiles with those of a similar control group who had tested negative. All who had tested positive, both asymptomatic and moderately symptomatic, retained a significant inflammatory response two months later with raised biomarkers, especially those related to anti-inflammatory responses and mitochondrial (the part of cells that produce energy) stress.
Salmon-Ceron et al. (2020) suggest Covid19 may lead to autoimmune conditions in genetically predisposed individuals. The British Society for Immunology (2020) observed that other viral infections can trigger a range of autoimmune diseases such as Guillain Barré syndrome. Yong's (2020) preprint notes that Long Covid can have similar symptoms to conditions such as lupus and rheumatoid arthritis. Dani et al. (2020) suggest Long Covid symptoms may be explained by ‘immune-mediated autonomic instability’ and may result in deconditioning (muscle weakness), hypovolaemia (low level of fluid in the body) or neuropathy (dysfunction of one or more nerves). They suggest that the symptoms of Long Covid are similar to orthostatic intolerance syndromes (inability to regulate blood pressure when changing position) including hypotension, fainting, tachycardia (racing heartbeat), palpitations, breathlessness and chest pain. This occurs when instead of blood vessels constricting when a person changes position (so blood doesn’t pool in the pelvis and legs), blood vessels dilate leading to low blood pressure, dizziness and ultimately fainting.
Viral persistence
Salmon-Ceron et al. (2020) reviewed people who had tested positive for Covid19 and whose symptoms had either lasted longer than two months from initial onset or had recurred. They found that 25% still had positive PCR nose and throat swabs. They suggest the virus may have continued to replicate in the colonised sites, or had spread to other parts of the body and in some cases, people had been infected with a different strain of Covid19. Landi et al. (2021) used PCR tests with patients discharged from an Italian hospital deemed to have recovered from COVID-19 and found 17% tested positive, however there was no difference in the prevalence of symptoms between patients with a negative test and those who tested positive. Referring to a number of other publications, Yong's (2020) preprint also reported that some patients still tested positive for Covid19 four months later. They also noted the virus has been detected in faeces for up to two months regardless of gastrointestinal symptoms. Yong's suggest that in certain cases, the viral persistence may lead to a specific immune response responsible for Long Covid symptoms.
Yeoh et al (2020) reviewed people who had tested positive for Covid19 and collected serial faeces samples up to 30 days after the virus was no longer detected. Gut microbiome (the type and range of microorganisms in the gut) was significantly altered compared with people who had not had Covid19 and was associated with inflammatory markers in the blood; they suggest the changes in the gut may contribute to Long Covid symptoms.
Evidence of cardiac and respiratory and other organ impairment
Puntmann et al. (2020) found 78% of people who were followed up around ten weeks after hospital discharge had abnormalities visible on cardiovascular magnetic resonance imaging and 60% had ongoing myocardial inflammation. Mandal et al. (2020) reported that 38% of patients in a Long Covid clinic had chest X-ray findings that remained abnormal and 9% had X-rays showing deterioration seven to eight weeks after discharge from hospital. Dennis et al. (2020) preprint reported on people thought to be at low risk from a Covid19 infection (82% of whom had not been hospitalised). 66% of those with ongoing symptoms had some degree of impairment in one or more organ systems four months after initial Covid19 symptoms. D’Cruz et al. (2020) used computerised tomography to scan the chests of patients with persistent respiratory symptoms and/or blood oxygen saturation levels dropping by more than 4% during a Sit to Stand test two months after being hospitalised for a severe Covid19 infection. 66% had some degree of impairment in one or more organ systems. 75% showed Covid19 related interstitial lung disease (tissue surrounding the airways) and/or airways disease.
Although there is evidence of organ impairment, it is too early to say whether it is reversible. However, organ impairment should be considered when investigating any Long Covid symptoms. Given Long Covid is a multiple system condition, impairment may be seen across a multiple organs, all of which may be related.
Thrombo embolism
There has been significant evidence of the impact of blood clotting in people hospitalised with Covid19 infections, with the introduction of anticoagulants for hospital patients being an early treatment success. There is some emerging evidence that thrombo embolism is a feature of people with Long Covid symptoms. Mandal et al. (2020) found 30% of people who had abnormal biomarkers when discharged from hospital had persistently elevated D–dimer levels (a test used to help diagnose clotting) and 10% had raised levels of C-reactive protein (CRP, which measures inflammation) eight weeks later. Venturelli et al. (2021) reported 17% of patients followed up after hospital discharge had D-dimer values twice the threshold for diagnosis of pulmonary embolism three months after they first tested positive for Covid19. Kommoss et al. (2020) noted that microvascular damage may also be a cause of persistent lung damage in patients with enduring symptoms. Vlachou et al. (2021) found the risk for pulmonary thrombosis remains raised least up to four weeks after discharge from hospital.
Biological sex
It has been widely acknowledged that there is a higher prevalence of men requiring critical care support and men have higher mortality rates from Covid19. Takahasksi and Iwasaki (2021) suggest biological sex differences in immunity may contribute to this, although this has not been tested in practice. Conversely, Karlsson et al. (2020) note the higher incidence of Long Covid in females and question whether the different T cell responses between males and females is responsible for Long Covid, through similar mechanisms to those that are known to lead to other autoimmune or inflammatory conditions which are higher in females.
Neurological impact
Wildwing and Holt’s (2021) overview of systematic review of neurological symptoms in Covid19 reported two types of neurological symptoms; life threatening symptoms such as Guillain Barré Syndrome and encephalitis, and chronic symptoms such as fatigue and myalgia which appear very similar to other neurological conditions such as Chronic Fatigue Syndrome (CFS) and Functional Neurological Disorder (FND). Baig (2020) suggests that Covid19 invokes different immune responses at different phases of the disease. They hypothesise that vascular events causing neurological problems are more common in the severe acute phase, whereas neurological symptoms of Long Covid are a result of either a low grade ‘smouldering’ inflammatory response and/or damaged nerve cells. Guedj et al. (2021) reviewed positron emission tomography (PET) scans of the brains of people with Long Covid more than three weeks after their initial infection and compared them with healthy matches. They found biomarkers consistent with memory and cognitive impairment and autonomic dysfunction that are seen in other diagnoses.
Psychological aspects
Using a validated hospital anxiety and depression scale, Tomasoni et al. (2020) found that 30% of people had anxiety and/or depression between one and three months after clearance of the Covid19 virus. These psychological conditions were not statistically related to gender or age. The British Psychological Association (2020) guidance on meeting the psychological needs of people recovering from severe coronavirus (Covid-19) suggest a range of symptoms may be seen and recommends psychological components of care to aid recovery.
Whilst a number of researchers refer to the psychological needs of people with Long Covid, this does not mean that there is no underlying and/or overlapping physical mechanisms and the psychological response to critical illness is well documented in post intensive care syndrome. Saying the cause of symptoms is not yet understood is not synonymous with saying there is no physical cause and the uncertainty around different classifications of Long Covid means a physical cause should be fully investigated. We know from other long-term physical conditions (such as heart failure and lung disease) that adjusting to changed health status can lead to depression and anxiety. The National Collaborating Centre for Mental Health (2018) asserted that two-thirds of people with a long-term condition will also have a mental health problem, mostly depression and anxiety disorders.
Impact of Long Covid on daily living
As well as clinical needs, the functional impairment seen in some people with Long Covid may result in community and social care needs. Our survey asked about other social impacts and 71% said Long Covid was affecting family life and relationships with 39% saying it was impacting their ability to care for their children or other dependents.
Cognitive difficulties and ‘brain fog’
A frequently reported symptom is ‘brain fog’. Hampshire et al. (2020) preprint analysed cognitive test data from 84,285 self-selected Great British Intelligence Test participants. To avoid bias, promotional material did not mention Covid19. Instead, people were told they could undertake a free online assessment to identify their cognitive strengths. After the assessment they were asked to complete a questionnaire regarding suspected and confirmed Covid19 infection. People who had recovered from Covid19 exhibited significant cognitive deficits when compared against controls. This was particularly so for people who had been hospitalised, but was also evident in non-hospitalised cases including those who reported no breathing difficulty. Cognitive difficulties were not explained by differences in age, education or other demographic and socioeconomic variables. The authors reported that problems demonstrated by those who were not ill enough to be admitted to hospital was unexpected.
Vaes et al. (2020) asked members of a Belgian Long Covid Facebook group who had not been admitted to hospital to complete the validated Care Dependency Scale (CDS). The scale asks 15 questions about activities of daily living such as personal care, household activities, and social and recreational activities. Only 8% of respondents reported that they had needed help with personal care before the onset of their Covid19 infection, but this increased to 52% 11 weeks after the infection, with 31% meeting the threshold for being care-dependent. Venturelli et al. (2021) reported that 18% of people who recalled having been totally independent prior to infection had some degree of dependency on others (defined by the Barthel Index) three months after hospital discharge.
One area of note is the impact on employment. In our survey, 67% of respondents were aged between 25 and 55 and 81% had been in paid employment at the time they became ill. 80% said it had affected their ability to work with 36% saying their symptoms were affecting their financial status. Similarly, Davis et al. (2020) preprint paper found 45% of those who did not recover within three month reported needing a reduced work schedule, and 22% were not working six months later. Halpin et al. (2021) reported that 15% of working people were off sick when followed up four to six weeks after discharge from hospital (rising to 38% in those who had an ICU admission).
Key points
Long Covid’s development is not predicted by initial Covid 19 severity. There is no clear evidence or clinical consensus about the cause of Long Covid. We do not know whether symptom patterns reflect already known syndromes or a unique new disease of Long Covid. For some, the physical, psychological and social impact can be severe.
Diagnosing and predicting the course of Long Covid
In our first review, we reported how people who have enduring symptoms often did not feel believed. Being able to predict those at higher risk of developing Long Covid would be helpful. We could not find reliable evidence for Long Covid risk factors, although we note that the ONS plans to capture data that will help.
Investigation and Diagnosis
Dennis et al. (2020) preprint paper on low-risk people who had had Covid19 (82% of whom had not been hospitalised) found 66% had some degree of impairment in one or more organ systems persisting for three to four months. However, the damage was more prevalent in those who had been admitted to hospital. Raman et al. (2021) studied patients between two and three months after discharge from hospital and compared them to matched controls as part of the PHOSP COVID study. The Covid19 positive patients reported higher rates of symptoms than the controls, and MRI scans showed abnormalities in their lungs (60%), heart (26%), liver (10%) and kidneys (29%). Whilst abnormalities were more frequent in people who had been most severely ill, even patients who were not ventilated or did not receive vasopressor/ionotropic support or renal replacement therapy showed evidence of organ impairment.
Similarly, Townsend et al. (2020) found no association between Covid19 severity (defined as need for inpatient admission, supplemental oxygen or critical care) and fatigue following Covid19. Additionally, there was no association between routine laboratory markers of inflammation and cell turnover and fatigue after Covid19.
D’Cruz et al. (2020) concluded that chest X-rays two months after discharge are a poor marker of disease damage. Only 13% of people in their study had evidence of Covid19 related lung disease on X-ray, but 46% reported higher breathlessness scores (compared with a pre-infection baseline), and 75% of those who went on to have CT scans were seen to have interstitial lung disease and/or airways disease. Dennis et al. (2020) preprint also concluded that symptoms and blood tests were not good predictors of organ damage. Current risk prediction models may not accurately reflect long-term morbidity. This may explain Arnold et al. (2020) finding that although 74% of people in their study had persistent symptoms, notably breathlessness and excessive fatigue and limited physical ability, chest X rays and spirometry only showed lung abnormalities in 35%.
Risk of deterioration
Moreno-Perez et al. (2020) found that neither baseline features, (age, sex, comorbidities) nor the symptoms of the initial disease predicted the development of post-Covid (Long Covid) syndrome. The only associations they found were for people with severe pneumonia, in whom higher heart rate and more lung abnormalities on admission to hospital were associated with Long Covid. They concurred with Amenta et al. (2020) that Long Covid symptoms can be subdivided into residual symptoms, organ dysfunction and new inflammatory symptoms, the implication being that they may have different predictors and require different diagnostic tests.
Barker Davies and colleagues (personal communication of a forthcoming paper) studied 155 service personnel referred to the UK Defence Medical Rehabilitation Centre following a Covid19 infection report. They found no relationships between acute symptoms or the location of care (home/hospital ward/ITU) and the need for post-Covid (Long Covid) rehabilitation. Indeed, people with delayed assessment (who were more likely to have stayed at home with their initial infection) were more likely to experience shortness of breath, pain and anxiety/mood disturbance than those with an early referral. The authors recommend prompt referral for all patients (including people who were not hospitalised and/or did not have confirmed infections) as there may be potential for deterioration in people finding difficulties accessing rehabilitation.
Ayoubkhani et al. (2021) preprint reported an ongoing ONS study that compared 47,780 individuals discharged from hospital after a Covid19 infection with controls matched for demographic and clinical characteristics. This showed higher rates of multi-organ damage across all ages and ethnicities. People discharged from hospital following a Covid19 infection were 3.5 times more likely to be readmitted and 7.7 times more likely to die within 140 days than controls. The risks of readmission was greater for people under 70 than those over 70 years, and for ethnic minority groups than for the white population. Similarly, Mandal et al. (2020) reported that 9% of patients in a Long Covid clinic had X-rays showing deterioration seven to eight weeks after discharge from hospital.
Key points
The continuing uncertainty about the aetiology of Long Covid means that it is difficult to predict who will experience severe consequences from it. All people reporting enduring symptoms associated with a confirmed or suspected Covid19 infection should receive a full assessment.
Management of Long Covid
The uncertainties around the causes of Long Covid, have meant that management has focused primarily on ruling out other diagnoses, treating individual symptoms and providing functional rehabilitation. Interventions have drawn on expert consensus and evidence from other conditions. We could not find any interventional studies evaluating the treatment of people with Long Covid.
Access to services has been variable. Humphreys et al. (2020) preprint explored the experience of people living with Long Covid and found some unable to access advice from health professionals about managing their conditions. In our survey, 15% of respondents with Long Covid had not sought any healthcare advice and a further 32% had not been able to access all of the healthcare they thought they needed. GP practices were the most frequently accessed service, with 37% of respondents saying they listened and helped them develop a management plan. 49% said that although they were sympathetic, GPs were not able to offer much help. Only 16% had accessed a psychologist or mental health service and only 11% had seen a physiotherapist.
The complexity of needs in some people with Long Covid mirrors the needs of people with multiple long-term conditions who benefit from a holistic, integrated approach rather than symptom by symptom management. Many people with Long Covid complain of fragmented care and 23% of our survey respondents wanted a case worker/key worker to co-ordinate care. Dennis et al. (2020) preprint concluded that care should be multidisciplinary. 77% of our survey respondents wanted a one-stop Covid clinic.
Rehabilitation
The Stanford Hall expert consensus statement (Barker-Davies et al. 2020) provides a framework of likely requirements of multidisciplinary rehabilitation for previously active individuals post Covid19, based on evidence from other conditions and professional expertise. The framework provides recommendations for rehabilitation of pulmonary, cardiac, musculoskeletal and neurological consequences of Covid19. It recommends all patients requiring rehabilitation following Covid19 have a functional assessment and those with post-intensive care syndrome should receive psychological, physical and cognitive rehabilitation. The Defence Medical Rehabilitation Centre at Stanford Hall is currently running a two week residential intervention and a concurrent research study to evaluate the programme.
There is evidence that pulmonary rehabilitation in the form of breathing exercises reduces breathlessness in chronic obstructive airways disease (Gloeckl et al. 2018; Hsieh et al. 2018) and Yong's (2020) preprint infers that it should work for respiratory symptoms in Long Covid.
Physical activity
A key element of rehabilitation is exercise. Exercise produces supercompensation to make the body stronger, but individuals have different levels of exercise tolerance. Rehabilitation exercise therefore needs careful prescription and monitoring.
The use of exercise as a therapy in Long Covid is contested. On one hand, many have noted the similarities between some of the symptoms of Long Covid and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) which can include exercise intolerance. Studies of SARS survivors raised concerns that exercise intolerance may persist for months after infection and Raman et al. (2020) found exercise intolerance correlated with markers of systemic inflammation. Many of the patients in Raman’s study stopped Cardio Pulmonary Exercise Testing (CPET) early because of generalised muscle ache and fatigue rather than breathlessness. In July 2020 NICE made a statement on its website that it should not be assumed that the recommendations on graded exercise therapy in its 2007 guideline on ME/CFS (CG53) apply to people with fatigue following Covid19. NICE issued a new draft guideline on ME/CFS for consultation in November 2020, recommending that exercise should be personalised and overseen by a physiotherapist or occupational therapist with specialist training and expertise. It recommends that fixed incremental increases in physical exercise, for example graded exercise therapy, should not be used.
On the other hand, physical activity is a well-established rehabilitation intervention for people who have become deconditioned, including those who have been bed ridden for some time. Whilst exercise should be approached with caution in ME/CFS, it may be helpful in other viral conditions, for example a systematic review of exercise and cognitive function in people living with HIV (Quigley et al. 2019) suggested that physical activity may preserve or improve cognition, although none of the studies were interventional and further research is needed.
Exercise tolerance/intolerance should not be seen as binary concept. A better term might be “symptom-titrated physical activity”. Using the term physical activity instead of exercise therapy also highlights the need to think about exercise as part of a person’s day to day life and the need to pace all activity. Pacing has parallels with elite athletes who cannot train to their maximum every day of the week and need to plan when to fit in the most demanding session and the lighter activity to complement it. When athletes train too hard or with inadequate rest they suffer from overtrain syndrome (OTS), which has symptoms similar to Long Covid; fatigue, depression, tachycardia, insomnia, irritability, hypertension, anxiety, weight loss and myalgia. There are a number of suggestions about the cause of OTS including autonomic dysregulation, increased inflammatory cytokines and dysregulation of the hypothalamus (Kreher and Schwartz 2012) and these mechanisms have also been proposed for Long Covid syndromes. Cadegiani and Kater (2019) recognised that OTS may be triggered by other mechanisms and have suggested a better name is “paradoxical deconditioning syndrome”.
The contradictory views on exercise underline that ongoing symptoms following a Covid19 infection may indeed represent different syndromes. Identifying whether patients have difficulties with breathlessness due to deconditioning (such as might be seen in post-intensive care syndrome) or to some other Long Covid syndrome is an important question (Mandel et al. 2020). Managing physical activity is complex with no ‘one size fits all’ recommendation. The Stanford Hall consensus (Barker Davies et al. 2020) highlighted the need to assess individual responses to exercise. It is clear that predicting which patients will need more time to recover between exercise sessions is difficult, especially in a novel condition like Long Covid. There may be a place for physical activity in Long Covid but the advantages and disadvantages need to be considered with an appropriately qualified practitioner and if exercise is deemed to be useful, a clinical review should be undertaken after each session.
Psychological care
Tabacof et al. (2020) preprint noted that unexplained and long lasting symptoms in Long Covid give rise to a sense of isolation. Like many others (e.g. Raman et al. 2020; Halpin et al. 2020; Moreno-Perez et al. 2020), they found that many people with Long Covid symptoms report lower quality of life scores.
It is well established that long-term physical health conditions can trigger psychological problems such as depression and anxiety (National Collaborating Centre for Mental Health, 2018) in addition to physical symptoms. In England, low-intensity interventions from trained practitioners (rather than clinical psychologists) have been offered to people with long-term conditions through the Improving Access to Psychological Therapies (IAPT) programme. Clark (2018) reported that 50% of people receiving IAPT recover and two-thirds show significant improvement. The service accepts both self-referrals and referrals from health professionals. Clark et al. (2009) found that self-referrals experienced symptoms for slightly longer than GP referrals, but were of similar need. There was a difference because a higher proportion of ethnic minority people came through self-referral than through GP referral.
Higher intensity psychological interventions from clinical psychologists are essential in multidisciplinary rehabilitation programmes, e.g. post-ICU, chronic-fatigue, chronic pain, cardiac and pulmonary rehabilitation programmes. The British Psychological Association Society (2020) produced expert consensus guidance on the psychological needs of people recovering from Covid 19 and recommended a structured, stepped approach to the psychological interventions as part of integrated, multidisciplinary rehabilitation. This has been incorporated into the NHS ‘Your Covid Recovery’ programme of psychological and physical aspects of rehabilitation. ‘Your Covid Recovery’ consists of an open access website and an App provided to patients by local healthcare teams to support their rehabilitation.
One of the frequently reported disabling symptoms of Long Covid is ‘brain fog’ or cognitive dysfunction. Whilst interventions to manage cognitive impairment in Long Covid have not been researched, it is a common feature of a number of neurological conditions including stroke and multiple sclerosis. McNicholas et al. (2018) report that cognitive dysfunction most commonly manifests as impaired information processing speed (the speed at which one can process verbal or visual information), working memory (the use of temporarily stored information for tasks such as reasoning) and verbal fluency.
Neuropsychology interventions aim to either restore the cognitive function, or if that is not possible, to aim for compensation by developing aids and new ways of organising information to ensure that the person is able to function. A 2014 Cochrane systematic review of neuropsychological rehabilitation in multiple sclerosis (Rosti-Otajärvi and Hämäläinen, 2014) found cognitive training combined with other neuropsychological rehabilitation methods improved attention, immediate verbal memory and delayed memory. A new Cochrane review is due to be published in 2021.
Self-management strategies
Programmes to build individuals’ knowledge, skills and confidence to manage their enduring symptoms are well established for long-term conditions and have been shown to improve outcomes (Bodenheimer et al. 2002). Online self-management tools work for some people but Van Hooft et al. (2016) systematic review found that programmes providing education only are the least successful and the support of a healthcare professional to develop personal strategies and motivating individuals is important. For example, Dani et al. (2020) emphasise the importance of working with people with orthostatic intolerance syndrome and how reproducing symptoms on a tilt table effective can help them to learn how to manage independently.
Key points
Long Covid is a broad term and can be a multi-system condition. People need investigation and, where indicated, specific clinical interventions. Some will require full rehabilitation programmes, and others may benefit from psychological services. Others will need long-term support in the community, including help with self-management strategies. The impact of Long Covid on vulnerable communities and pre-existing conditions has not been researched, and the long-term needs of these groups is unclear.
Conclusion
There is growing evidence about the enduring symptoms experienced by some people infected with Covid19. The pattern of the disease does not always follow that of a typical respiratory infection and the reasons for that are not clear, although it appears that individuals have different responses to the virus, as is also seen with initial infection when some remain well and asymptomatic and others become life-threateningly unwell. Estimates of Long Covid vary but it seems that at least 10% of all people who contract Covid19 have some symptoms for at least 12 weeks and as the pandemic continues, the number of people with Long Covid grows. Long Covid is seen in all age groups, but we did not see much evidence around how the needs may differ for the young (under 18) or the old (over 65). Nor do we understand how prevalent it is in ethnic minority populations.
Long Covid is a multi-system disease in some people, and a number of researchers have identified discrete patterns of symptoms. Further investigation into sub classifications of Long Covid might explain the variations in incidence and estimates of prevalence. More attention needs to be focused on the duration of symptoms, particularly the number of people still ill months and now a year later. The causes of Long Covid are complex and multifactorial and not well understood. There is emerging evidence that this is not a static condition and may deteriorate over time so early assessment and ongoing monitoring is important for all people with Long Covid symptoms
At present, the journey of Long Covid is not well understood and it is important to continue to listen to the lived experience as we move into the second year of this new disease. There is a significant need for more research.
Research Recommendations
- More research is needed on the incidence of Long Covid and its causes and this will help to predict and prevent Long Covid in the longer term. There is an urgent need to research treatments and management for people with Long Covid.
- The emergent nature of the understanding of Long Covid emphasises the need to continue to explore a range of hypotheses in any research that is undertaken.
- A precursor to research in all areas is a better understanding of the disease syndromes and symptom clusters that currently sit under the umbrella of Long Covid or post Covid.
- We recommend that a minimum data set for recording a wide range of symptoms be agreed and used by both researchers and healthcare providers.
- Some elements of Long Covid are similar to other conditions and evaluations of interventions (pharmaceutical, psychological and physical therapies) that may improve symptoms. For non-pharmaceutical interventions, a range of research methodologies should be encouraged.
- Long Covid is a significant health burden that is unlikely to be met by existing NHS services and new delivery models that allow rapid access are needed. We recommend rapid evaluation of different service models and skill mix for supporting people with Long Covid.
- Seldom heard voices are not visible in the current evidence. We recommend research that is targeted at vulnerable people (including older people and people with learning disabilities) as well as hard-to-reach groups including travellers and prison populations.
- We recommend that people living with Long Covid (who are experts by experience) should be equal partners in setting the research agenda.
How to cite this review
NIHR Themed Review: Living with Covid19 - Second review; March 2021; doi:10.3310/themedreview_45225
This review was written by Elaine Maxwell, Content Lead, NIHR , with Ruth Poole, Senior Healthcare Evaluation Scientist, Cedar Evaluation Centre, Cardiff. We would also like to acknowledge the contributions to the identification of literature by Pauline Oustric, PhD student in Biopsychology at University of Leeds and Co-founder of #ApresJ20 Association Covid Long, France.
The review was shaped by our Steering Group:
Group Captain Alex Bennett, Professor of Rheumatology and Rehabilitation Medicine, Defence Medical Rehabilitation Centre / Loughborough University
Squadron Leader Rob Barker-Davies, Defence Medical Rehabilitation Centre
Professor Roshan das Nair, Professor of Clinical Psychology and Neuropsychology, University of Nottingham
Caroline Morrice, CEO, Guillain Barré and Associated Inflammatory Neuropathies (GAIN)
Dr Hannah Murray, Research Clinical Psychologist, Oxford Centre for Anxiety Disorders and Trauma
Dr David Murphy Chair of COVID-19 Coordinating Group, British Psychological Society
Dr David Oliver, Geriatrician, Royal Berkshire NHS FT
Dr Philip Pearson, Respiratory Physician, Northampton General Hospital NHS Trust
Professor Sarah Tyson, Professor of Rehabilitation, University of Manchester
Tara Lamont, Senior Scientific Advisor, University of Southampton
Liz Jones, Policy Director, National Care Forum
Professor Julienne Meyer, R&D Advisor, National Care Forum
Dr Crystal Oldman, Chief Executive, Queen’s Nursing Institute
Dr Vanessa Abrahamson, Royal College of Occupational Therapists/University of Kent
Dr Jo House, representative from our Patient Reference Group
References
Barker-Davies, R.M., O’Sullivan, O., Senaratne, K.P.P., Baker, P., Cranley, M., Dharm-Datta, S., Ellis, H., Goodall, D., Gough, M., Lewis, S. and Norman, J., (2020) The Stanford Hall consensus statement for post-COVID-19 rehabilitation. British journal of sports medicine, 54(16), pp.949-959.
Bodenheimer T, Lorig K, Holman H, Grumbach K. (2002) Patient self-management of chronic disease in primary care. J Amer Med Assoc 20; 288(19):2469-75.British Society for Immunology (2020) Long-term immunological health consequences of COVID-19
Callard, F. and Perego, E., (2021). How and why patients made Long Covid. Social Science & Medicine, 268, p.113426.
Cadegiani, F.A. and C.E. Kater, Novel insights of overtraining syndrome discovered from the EROS study. BMJ open sport & exercise medicine, 2019. 5(1): p. e000542-e000542.
Clark, D.M., Layard, R., Smithies, R., Richards, D.A., Suckling, R. and Wright, B. (2009) Improving access to psychological therapy: Initial evaluation of two UK demonstration sites. Behaviour research and therapy, 47(11), pp.910-920.
Clark, D.M., (2018) Realising the mass public benefit of evidence-based psychological therapies: the IAPT program. Annual review of clinical psychology, 14, pp.159-183.
Fenton, W.S. and Stover, E.S., 2006. Mood disorders: cardiovascular and diabetes comorbidity. Current Opinion in Psychiatry, 19(4), pp.421-427.
Benton, T., Staab, J. and Evans, D.L., (2007) Medical co-morbidity in depressive disorders. Annals of Clinical Psychiatry, 19(4), pp.289-303.
Welch, C.A., Czerwinski, D., Ghimire, B. and Bertsimas, D. (2009. Depression and costs of health care. Psychosomatics, 50(4), pp.392-401.
Gloeckl, R., Schneeberger, T., Jarosch, I. and Kenn, K., (2018). Pulmonary rehabilitation and exercise training in chronic obstructive pulmonary disease. Deutsches Ärzteblatt International, 115(8), p.117.
Hsieh, M.J., Lee, W.C., Cho, H.Y., Wu, M.F., Hu, H.C., Kao, K.C., Chen, N.H., Tsai, Y.H. and Huang, C.C., (2018). Recovery of pulmonary functions, exercise capacity, and quality of life after pulmonary rehabilitation in survivors of ARDS due to severe influenza A (H1N1) pneumonitis. Influenza and other respiratory viruses, 12(5), pp.643-648.
Karlsson, A.C., Humbert, M. and Buggert, M., (2020) The known unknowns of T cell immunity to COVID-19. Science Immunology, 5(53).
Kreher, J.B. and J.B. Schwartz (2012) Overtraining Syndrome: A Practical Guide. Sports Health 4(2): p. 128-138.
Lam, M.H.B., Wing, Y.K., Yu, M.W.M., Leung, C.M., Ma, R.C., Kong, A.P., So, W.Y., Fong, S.Y.Y. and Lam, S.P. (2009) Mental morbidities and chronic fatigue in severe acute respiratory syndrome survivors: long-term follow-up. Archives of internal medicine, 169(22), pp.2142-2147.
McNicholas, N., O’Connell, K., Yap, S.M., Killeen, R.P., Hutchinson, M. and McGuigan, C., 2018. Cognitive dysfunction in early multiple sclerosis: a review. QJM: An International Journal of Medicine111(6), pp.359-364.
National Collaborating Centre for Mental Health (2018) The Improving Access to Psychological Therapies (IAPT) Pathway for People with Long-term Physical Health Conditions and Medically Unexplained Symptoms. Full implementation guidance. London
NICE (2020) https://www.nice.org.uk/guidance/ng188Statement about graded exercise therapy in the context of COVID-19
NICE (2007) Chronic fatigue syndrome/myalgic encephalomyelitis (or encephalopathy): diagnosis and management
NICE (2020) Guideline, Myalgic encephalomyelitis (or encephalopathy)/chronic fatigue syndrome: diagnosis and management. Draft for consultation, November 2020
NICE (2009) Depression in adults with a chronic physical health problem: recognition and management
ONS (2020) The prevalence of long COVID symptoms and COVID-19 complications
ONS (2021) Updated estimates of the prevalence of long COVID symptoms
Public Health England (7th September 2020) COVID-19: long-term health effects
Quigley, A., O’Brien, K., Parker, R. and MacKay-Lyons, M. (2019) Exercise and cognitive function in people living with HIV: a scoping review. Disability and rehabilitation, 41(12), pp.1384-1395
Rosti‐Otajärvi, E.M. and Hämäläinen, P.I., 2014. Neuropsychological rehabilitation for multiple sclerosis. Cochrane Database of Systematic Reviews (2).
Takahashi, T. and Iwasaki, A. (2021). Sex differences in immune responses. Science, 371(6527), pp.347-348.
van Hooft, S.M., Been‐Dahmen, J.M., Ista, E., van Staa, A. and Boeije, H.R., 2017. A realist review: What do nurse‐led self‐management interventions achieve for outpatients with a chronic condition? Journal of Advanced Nursing, 73(6), pp.1255-1271.
APPENDIX A: Research studies
Ayoubkhani, D., Khunti, K., Nafilyan, V., Maddox, T., Humberstone, B., Diamond, I. and Banerjee, A., (2021) *PREPRINT* Epidemiology of post-COVID syndrome following hospitalisation with coronavirus: a retrospective cohort study. medRxiv.
This retrospective matched cohort study reports findings from NHS Hospitals in England using routinely-recorded data from 47,780 people who had been discharged following an inpatient stay with a primary diagnosis of Covid19 (identified by laboratory testing or clinical criteria). This was compared with a general population comparator group from the same period, matched against demographics and clinical history. Post-discharge rates of multi-organ dysfunction were higher in those who had previously been admitted with acute Covid19 than those who had not, and nearly a third were readmitted. The relative risk of post-discharge adverse events (such as diabetes, kidney disease, lung disease, or cardiovascular events) was higher in people aged <70 years than in older patients, and also higher in non-white ethnic minority individuals when compared with those of white ethnic backgrounds. This paper has not yet been peer-reviewed.
Ahmed, M., Advani, S., Moreira, A., Zoretic, S., Martinez, J., Chorath, K., Acosta, S., Naqvi, R., Burmeister-Morton, F., Burmeister, F. and Tarriela, A. (2020) Multisystem inflammatory syndrome in children: A systematic review. EClinicalMedicine, 26, p.100527.
Multisystem inflammatory syndrome has been identified in children, typically presenting three or four weeks after initial infection with the Covid19 virus. This overview of available evidence is based on 39 observational studies (n=662). It describes the clinical presentation and signs and symptoms of Multisystem Infllammatory Syndrome in Children (MIS-C). The authors note that long-term outcomes are unknown.
Amenta, E.M., Spallone, A., Rodriguez-Barradas, M.C., El Sahly, H.M., Atmar, R.L. and Kulkarni, P.A., (2020) December. Postacute COVID-19: An Overview and Approach to Classification. Open forum infectious diseases (Vol. 7, No. 12, p. ofaa509).
This review discusses classification systems for distinguishing between different manifestations of ‘postacute’ Covid19. Methods for identifying and selecting relevant literature are not described. The authors propose three categories (which are not mutually exclusive): 1) persistent symptoms of infection; 2) organ dysfunction; and 3) multisystem inflammatory syndrome (MIS). They acknowledge that the duration, severity, and prevalence of postacute Covid19 is unknown, and that new syndromes may emerge as we better understand the mechanisms of organ dysfunction and how they are associated with symptomatology.
Arnold, D.T., Hamilton, F.W., Milne, A., Morley, A.J., Viner, J., Attwood, M., Noel, A., Gunning, S., Hatrick, J., Hamilton, S. and Elvers, K.T. (2020) Patient outcomes after hospitalisation with COVID-19 and implications for follow-up: results from a prospective UK cohort. Thorax
A primary observational cohort study at a single NHS centre in Bristol, UK. Consecutive patients admitted with Covid19 (confirmed by a positive PCR test result or clinical/radiological diagnosis) were prospectively recruited. All survivors who had been discharged from hospital were invited to an outpatient clinic review, and 110 people attended 8-12 weeks after their acute infection. Outcomes were based on medical review, physiological tests, chest imaging, and a quality of life questionnaire. Results were reported separately according to the severity of initial illness (mild, moderate or severe). The study investigators observed that those patients with mild Covid19 (not requiring supplemental oxygen) had a low likelihood of having abnormalities detected on chest x-ray at follow-up. However they did note that most participants (74%) reported at least one persistent symptom or limited physical ability, including those originally admitted with mild disease.
Baig, A.M., (2020) Deleterious Outcomes in Long-Hauler COVID-19: The Effects of SARS-CoV-2 on the CNS in Chronic COVID Syndrome. ACS chemical neuroscience.
This ‘viewpoint’ article discusses some potential pathogenic pathways and implications for long-term management of the neurological sequelae of Covid19. Hypotheses associated with pathogenesis of central nervous system disease at the molecular level include a low-grade inflammatory response, with or without degeneration of nerve cells and supporting tissues.
Bergamaschi, L., Mescia, F., Turner, L., Hanson, A., Kotagiri, P., Dunmore, B.J., Ruffieux, H., De Sa, A., Huhn, O., Wills, M.R. and Baker, S., (2021) *PREPRINT* Early immune pathology and persistent dysregulation characterise severe COVID-19. medRxiv.
The main focus of this study is on early mechanisms of pathological dysregulation in acute Covid19. 207 people who tested positive for Covid19 were recruited, ranging from people who were asymptomatic to people who were admitted to ITU. They performed detailed immune phenotyping at multiple time points up to 90 days from symptom onset. Variable recovery over three months is associated with marked changes in the nature of the systemic inflammation seen in severe Covid19. The paper adds to the evidence supporting a potential role of late immunometabolic inflammatory changes and unresolved immune cell defects in the development of ‘Long Covid’. This paper has not yet been peer-reviewed.
Buonsenso, D., Munblit, D., De Rose, C. Sinatti, D., Ricchiuto, A. Carfi, A., Valentini, P (2021) *PREPRINT* Preliminary Evidence on Long COVID in children. medRxiv
This cross-sectional study in Italy prospectively recruited 129 children with laboratory-confirmed Covid19. Interviews with caregivers indicated persistence of one or more symptoms in 53% children 120 days after Covid19 diagnosis, with 43% reporting an impact on activities of daily living. The authors intend to continue monitoring of this group of children, and to compare findings with a control group (not having been diagnosed with Covid19). This paper has not yet been peer-reviewed.
Carfì, A., Bernabei, R. and Landi, F. (2020). Persistent symptoms in patients after acute COVID-19. Jama, 324(6), pp.603-605.
In one of the first clinical reports on symptoms of Long Covid, Carfi et al. (2020) describe outcomes from a post acute outpatient service for people discharged from an Italian hospital after Covid19. In addition to medical examination, 143 patients were asked to retrospectively reflect on which symptoms they had experienced during their acute illness, and whether those symptoms had continued until the follow-up appointment (on average around two months after symptom onset). A high proportion (87%) reported persistence of at least one symptom. The study was limited by a lack of detail on the symptoms and severity early in the patients’ experience.
Ceravolo, M.G., Arienti, C., De Sire, A., Andrenelli, E., Negrini, F., Lazzarini, S.G., Patrini, M. and Negrini, S. (2020) Rehabilitation and COVID-19: the Cochrane Rehabilitation 2020 rapid living systematic review. Eur J Phys Rehabil Med, pp.642-651.
This Cochrane Collaboration review sought to inform the rehabilitation of patients with Covid19, including activities undertaken before hospital discharge, as well as rehabilitation in other settings. The authors searched the literature for primary research papers, without restricting the search according to study design. Thirteen studies focused on the immediate ‘post-acute’ phase – typically reporting findings up to one month after discharge. No study reported data concerning permanent sequelae or late-onset complications.
Cirulli, E., Barrett, K.M.S., Riffle, S., Bolze, A., Neveux, I., Dabe, S., Grzymski, J.J., Lu, J.T. and Washington, N.L. (2020) *PRE PRINT* Long-term COVID-19 symptoms in a large unselected population. medrxiv.
Participants in two existing US cohort studies were invited to respond to a series of surveys, regardless of their Covid19 status. Of the 24,949 respondents, 357 had tested positive for Covid19, 5,497 tested negative, and 19,095 had not been tested. Most of those with Covid19 had mild acute illness not requiring hospital admission, and were thought to be representative of the general population. After 30, 60, and 90 days respondents selected their ongoing symptoms from a list of 32 (those thought to be associated with Covid19 or Long Covid). The investigators reported the proportions of those who had one or more symptoms at each time interval, as well as a subgroup who had more than five symptoms. In statistical analysis, Covid19 positive patients had the highest prevalence of continuing symptoms at each of the three timepoints when compared with both those who had tested negative, and those who had not been tested. This paper has not yet been peer-reviewed.
Dani, M., Dirksen, A., Taraborrelli, P., Torocastro, M., Panagopoulos, D., Sutton, R. and Lim, P.B. (2021) Autonomic dysfunction in ‘long COVID’: rationale, physiology and management strategies. Clinical Medicine, 21(1), p.e63.
Six women presenting with orthostatic intolerance, all of whom were suspected of previously having survived a debilitating Covid19 episode (though only one had a confirmatory test result). It was hypothesised that some of the symptoms of Long Covid result from a virus- or immune-mediated disruption of the autonomic nervous system. The autonomic instability may also be exacerbated as a consequence of hypovolaemia (during initial infection) or deconditioning (after prolonged bed-rest). Corresponding management strategies are suggested.
Davis, H.E., Assaf, G.S., McCorkell, L., Wei, H., Low, R.J., Re’em, Y., Redfield, S., Austin, J.P. and Akrami, A., (2020) *PREPRINT* Characterizing Long COVID in an International Cohort: 7 Months of Symptoms and Their Impact. medRxiv.
In a patient-led study, an international survey was distributed via online support groups and social media. It collected data from 3,762 people who had ongoing symptoms at least 28 days after confirmed (27%) or suspected Covid19 infection. More than 200 symptoms of varying severity were reported, with some lasting seven months or more, and sometimes following a relapsing-remitting trajectory. Survey respondents describe the disabling nature of their condition, with many feeling unable to return to previous levels of work even after six months. The authors note similarities between some of the symptoms of Long Covid and other conditions, including: Postural Orthostatic Tachycardia Syndrome (POTS); Myalgic Encephalitis/Chronic Fatigue Syndrome (ME/CFS); and Mast Cell Activation Syndrome (MCAS). The study design does not enable estimation of symptom prevalence at a population level, given the self-selected sample and absence of denominators. This paper has not yet been peer-reviewed.
D'Cruz, R.F., Waller, M.D., Perrin, F., Periselneris, J., Norton, S., Smith, L.J., Patrick, T., Walder, D., Heitmann, A., Lee, K. and Madula, R., (2020). Chest radiography is a poor predictor of respiratory symptoms and functional impairment in survivors of severe COVID-19 pneumonia. ERJ Open Research.
This single-centre observational cohort study focused on radiological outcomes from 119 patients with severe Covid19 pneumonia, when assessed four to six weeks after discharge after discharge from a UK hospital. These patients commonly exhibited persistent symptoms, adverse mental health outcomes, and physiological impairment, despite radiological resolution of Covid19 pneumonitis in 87%.
Dennis, A., Wamil, M., Kapur, S., Alberts, J., Badley, A., Decker, G.A., Rizza, S.A., Banerjee, R. and Banerjee, A., (2020) *PREPRINT* Multi-organ impairment in low-risk individuals with long COVID. medrxiv.
The Coverscan study aims recruit around 500 participants to map the prevalence and impact of Covid19 on multiple organs using magnetic resonance imaging (MRI), blood DNA tests, and online questionnaires. This is an interim report of patients with ongoing symptoms who were recovering after (a confirmed diagnosis of) Covid19 Those recruited were young (average 44 years) and had relatively few pre-existing conditions. Of 201 participants reported to date, only 18% had been hospitalised during their acute illness. Despite demographic characteristics suggesting low risk from Covid19, mild organ impairment was detected in the heart (32%), lungs (33%), kidneys (12%), liver (10%), pancreas (17%), and spleen (6%). Organ impairment was significantly associated with risk of prior Covid19 hospitalisation. This paper has not yet been peer-reviewed.
Doykov, I., Hällqvist, J., Gilmour, K.C., Grandjean, L., Mills, K. and Heywood, W.E. (2020) ‘The long tail of Covid-19’-The detection of a prolonged inflammatory response after a SARS-CoV-2 infection in asymptomatic and mildly affected patients. F1000Research, 9.
Proteins from serum samples of 20 healthcare workers, 10 of whom had tested positive for Covid19 and 10 of whom had tested negative were analysed using a multiplex assay. The immune profiles of the people who had tested positive for Covid19 (but had not been hospitalised) were clearly disrupted even 40 days after infection, when compared those of who had tested negative. The biomarker proteins which had been significantly altered were either anti-inflammatory or associated with a stress response.
Guedj, E., Campion, J.Y., Dudouet, P. et al. (2021) 18F-FDG brain PET hypometabolism in patients with Long COVID. Eur J Nucl Med Mol Imaging.
Three weeks after confirmed Covid19 infection, Long Covid patients report functional complaints of possible neurological origin (such as shortness of breath, insomnia, pain, or cognitive impairment). Positron Emission Tomography (PET) scan data from 35 patients was retrospectively matched with healthy controls for age and sex. Clusters of hypometabolism were detected in specific areas of the brain which were associated with the patients’ symptoms and functional complaints. An increased number of functional complaints correlated with a longer duration since initial symptoms (which ranged from 26 to 155 days). Interestingly, memory/cognitive impairment and an increased number of functional complaints also correlated with younger age. The study authors propose that the functional complaints could involve a systemic immune-inflammation disorder, possibly in association with psychological factors.
Halpin, S.J., McIvor, C., Whyatt, G., Adams, A., Harvey, O., McLean, L., Walshaw, C., Kemp, S., Corrado, J., Singh, R. and Collins, T., (2021) Postdischarge symptoms and rehabilitation needs in survivors of COVID‐19 infection: A cross‐sectional evaluation. Journal of medical virology, 93(2), pp.1013-1022.
This publication from early in the pandemic describes symptoms and impact on daily life 4-8 weeks after UK hospital discharge, in a purposively sampled group of 100 Covid19 survivors (who had been diagnosed using a PCR swab test). Prevalence of Long Covid symptoms was higher in those who required ICU care when compared with those who were managed on the ward. A clinically significant reduction in quality of life was found in 69% of the ICU group, and 46% of the ward group.
Hampshire, A., Trender, W., Chamberlain, S., Jolly, A., Grant, J.E., Patrick, F., Mazibuko, N., Williams, S., Barnby, J.M., Hellyer, P. and Mehta, M.A., (2020)*PREPRINT* Cognitive deficits in people who have recovered from COVID-19 relative to controls: An N= 84,285 online study. MedRxiv.
This large scale cross-sectional study (n=84,285) provides insights into how cognitive deficits (such as issues with memory, attention, or problem-solving) may be associated with Long Covid. Members of the general public – largely based within the UK – were invited to take part in the Great British Intelligence Test. In May 2020 this existing online tool was expanded to include questions about Covid19, including antigen test results, and related symptoms. The researchers found that people who had recovered from confirmed or suspected Covid19 performed significantly worse on cognitive tests than the general population, even after controlling for demographic profiles. This paper has not yet been peer-reviewed.
Huang, C., Huang, L., Wang, Y., Li, X., Ren, L., Gu, X., Kang, L., Guo, L., Liu, M., Zhou, X. and Luo, J., (2021) 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. The Lancet.
Researchers in Covid19 in Wuhan, China, have access to longer-term follow-up data than those elsewhere. This large cohort study (n=1,733) reports long-term physical, psychological and clinical outcomes in patients discharged from a hospital in Wuhan province. Severe acute illness was associated with detection of abnormalities on chest imaging and impaired lung function after six months.
Humphreys, H., Kilby, L., Kudiersky, N. and Copeland, R., (2020) *PRE PRINT* Long Covid and the role of physical activity: a qualitative study. medRxiv.
Eighteen people (17 from the UK and 1 from the US) participated in semi-structured telephone interviews, to qualitatively explore their lived experience with Long Covid. Four main themes emerged: 1) Physical, social and medical isolation; 2) Seeking validation and answers; 3) Learning how to balance symptoms and activity; 4) Adapting to an altered life. This paper has not yet been peer-reviewed.
Kommoss, F.K., Schwab, C., Tavernar, L., Schreck, J., Wagner, W.L., Merle, U., Jonigk, D., Schirmacher, P. and Longerich, T., 2020. The Pathology of Severe COVID-19-Related Lung Damage: Mechanistic and Therapeutic Implications. Deutsches Ärzteblatt International, 117(29-30), p.500.
Autopsies were carried out on 13 people who had died of Covid19. The cause of death in most patients was lung damage, apparently caused by small blood clots in the small blood vessels that supply the tiny sacs where gas exchange takes place. The authors suggest that this could also be a mechanism that also affects some people who survive Covid19, with pulmonary fibrosis leading to impairment of lung function. No pathological changes in other organs were detected.
Landi, F., Carfì, A., Benvenuto, F., Brandi, V., Ciciarello, F., Monaco, M.R.L., Martone, A.M., Napolitano, C., Pagano, F., Paglionico, A. and Petricca, L.,(2021) Predictive factors for a new positive nasopharyngeal swab among patients recovered from covid-19. American Journal of Preventive Medicine, 60(1), pp.13-19.
People who had been declared ‘recovered’ from a hospital admission with confirmed Covid19 in Rome, Italy were enrolled into a study through a post-acute care service. Recovery was defined according to WHO criteria for discontinuation of quarantine (including a requirement for two negative test results at least 24 hours apart). Of 131 patients who underwent a follow-up PCR test around two months after initial disease onset, 17% tested positive again. Persistent symptoms were reported by a large proportion of patients, regardless of whether or not their follow-up result was positive or negative.
Logue, J.K., Franko, N.M., McCulloch, D.J., McDonald, D., Magedson, A., Wolf, C.R. and Chu, H.Y. (2021) Sequelae in adults at 6 months after COVID-19 infection. JAMA Network Open 4(2), pp.e210830-e210830
A longitudinal cohort study of 177 US adults with laboratory-confirmed Covid19 (16 of whom had been hospitalised). Data from a concurrent control group were also available, but statistical comparisons were not carried out due to small sample sizes (although descriptive data are reported). Participants were asked to complete a single follow-up questionnaire between three and nine months of symptom onset (averaging around five to six months). Impact on activities of daily living and on quality of life was assessed, and around 30% of both hospitalised and non-hospitalised people reported Long Covid symptoms (despite most having experienced mild acute illness).
Ludvigsson, J.F. (2020) Case report and systematic review suggest that children may experience similar long‐term effects to adults after clinical COVID‐19. Acta Paediatrica.
Although Ludvigsson attempted to carry out a systematic review, none of the identified papers reported on Long Covid in children. Instead the author relies on case reports from five children in Sweden. Their parents described symptoms six to eight months after clinical diagnosis, which appeared to be similar to the symptoms reported by adults with Long Covid.
Mandal, S., Barnett, J., Brill, S.E., Brown, J.S., Denneny, E.K., Hare, S.S., Heightman, M., Hillman, T.E., Jacob, J., Jarvis, H.C. and Lipman, M.C. (2020) ‘Long-COVID’: a cross-sectional study of persisting symptoms, biomarker and imaging abnormalities following hospitalisation for COVID-19. Thorax.
Around two months (on average) after discharge from any of three London hospitals, 384 Covid19-positive patients were followed up by telephone or in person to enquire about persistent symptoms. At the time of discharge some had abnormalities detected in blood test or scan results; this subgroup was invited to undergo repeat testing. Of 229 patients who underwent follow-up blood tests, 30% had elevated D-dimer biomarkers. 224 patients had follow-up radiographs, with 9% showing significant post-discharge deterioration suggestive of pulmonary fibrosis.
Munblit, D., Bobkova, P., Spiridonova, E., Shikhaleva, A., Gamirova, A., Blyuss, O., Nekliudov, N.A., Bugaeva, P., Andreeva, M., DunnGalvin, A. and Comberiati, P. (2021) *PRE PRINT* Risk factors for long-term consequences of COVID-19 in hospitalised adults in Moscow using the ISARIC Global follow-up protocol: StopCOVID cohort study. medRxiv.
A longitudinal cohort study (StopCOVID) collected follow-up data from 2,649 adults discharged from a Russian hospital after clinical or laboratory diagnosis of Covid19. Around six to eight months after initial infection, 47% reported at least one Long Covid symptom. Clusters of symptoms were identified, with 11% of people exhibiting multi-system involvement (affecting three or more categories of symptoms). This paper has not yet been peer-reviewed.
Moreno-Pérez, O., Merino, E., Leon-Ramirez, J.M., Andres, M., Ramos, J.M., Arenas-Jiménez, J., Asensio, S., Sanchez, R., Ruiz-Torregrosa, P., Galan, I. and Scholz, A. (2021) Post-acute COVID-19 Syndrome. Incidence and risk factors: a Mediterranean cohort study. Journal of Infection.
This prospective cohort study recruited 277 adults with Covid19 (confirmed by antigen or antibody testing), who had recovered 10 to 14 weeks after symptom onset. All had initially presented with acute illness at an Emergency Department in Spain, then subsequently managed in hospital (66%), primary care (20%), or at home (15%). At follow-up, Long Covid symptoms were reported by 51% of people. Mild abnormalities were detected on 19% of radiographs and 9% of spirometry breathing tests.
Puntmann, V.O., Carerj, M.L., Wieters, I., Fahim, M., Arendt, C., Hoffmann, J., Shchendrygina, A., Escher, F., Vasa-Nicotera, M., Zeiher, A.M. and Vehreschild, M., (2020) Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA cardiology, 5(11), pp.1265-1273.
This prospective German cohort study looked at the cardiovascular effects of Covid19 using magnetic resonance imaging (MRI) in 100 ‘unselected’ people who had tested positive and then recovered for an average of 71 days after hospitalisation (33%) or management at home (67%). Cardiac involvement was found in 78%, with 60% exhibiting ongoing myocardial inflammation.
Raman, B., Cassar, M.P., Tunnicliffe, E.M., Filippini, N., Griffanti, L., Alfaro-Almagro, F., Okell, T., Sheerin, F., Xie, C., Mahmod, M. and Mózes, F.E.,(2021). Medium-term effects of SARS-CoV-2 infection on multiple vital organs, exercise capacity, cognition, quality of life and mental health, post-hospital discharge. EClinicalMedicine, 31, p.100683.
Around two to three months after onset of symptoms, outcomes from 58 patients hospitalised with Covid19 in the UK were compared with matched controls. Patients had impairment of quality of life and a higher burden of self-reported depression. MRI scans indicated multi-organ damage, with impaired cognitive functioning and reduced exercise tolerance.
Salmon-Ceron, D., Slama, D., De Broucker, T., Karmochkine, M., Pavie, J., Sorbets, E., Etienne, N., Batisse, D., Spiridon, G., Le Baut, V. and Meritet, J.F. (2020) Clinical, virological and imaging profile in patients with prolonged forms of COVID-19: A cross-sectional study. The Journal of infection.
Salmon-Ceron and colleagues report findings from a Paris outpatient clinic for adults with persistent and/or recurrent symptoms after testing positive for Covid19 antigens or antibodies. Characteristics of late symptoms were described for 70 consecutive patients, accompanied by speculative hypotheses about pathogenic mechanisms. Only 9% had been hospitalised during acute illness. Phases are described in which symptoms persisted, disappeared and reappeared, or presented for the first time.
Sudre, C.H., Murray, B., Varsavsky, T., Graham, M.S., Penfold, R.S., Bowyer, R.C., Pujol, J.C., Klaser, K., Antonelli, M., Canas, L.S. and Molteni, E. (2020) *PRE PRINT* Attributes and predictors of Long-COVID: analysis of COVID cases and their symptoms collected by the Covid Symptoms Study App. medRxiv.
The Covid Symptoms Study (‘Zoe’) app collected self-reported symptom data from a subset of 4,182 participants with Covid19 positive tests. Comparisons were made with matched symptomatic test-negative controls. Findings were characterised according to different periods of follow-up: up to 28 days, eight weeks or more, and those persisting for at least 12 weeks. Two main patterns of symptomatology were identified. This paper has not yet been peer-reviewed.
Tabacof, L., Tosto-Mancuso, J., Wood, J., Cortes, M., Kontorovich, A., McCarthy, D., Rizk, D., Nasr, L., Breyman, E., Mohammadi, N. and Kellner, C. (2020) *PREPRINT* Postacute COVID-19 syndrome negatively impacts health and wellbeing despite less severe acute infection. medRxiv.
Cross-sectional observational survey data from 84 patients referred to a US recovery programme were retrospectively analysed. Participants had either a confirmed or suspected history of acute Covid19, and continued to experience symptoms at least six weeks after onset. They are described as “previously healthy, relatively young adults”; only a small proportion had been admitted to hospital. Despite a mild initial illness, symptoms persisted for an average of at least 5 months and were associated with increased disability and reduced quality of life. This paper has not yet been peer-reviewed.
Tenforde, M.W., Kim, S.S., Lindsell, C.J., Rose, E.B., Shapiro, N.I., Files, D.C., Gibbs, K.W., Erickson, H.L., Steingrub, J.S., Smithline, H.A. and Gong, M.N. (2020) Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. Morbidity and Mortality Weekly Report, 69(30), p.993.
292 adults who had previously tested positive for Covid19 at a US outpatient clinic were followed up in a telephone interview around two weeks later. Of 274 interviewees who had experience symptoms when initially tested, 35% reported that they had not returned to their usual state of health.
Tomasoni, D., Bai, F., Castoldi, R., Barbanotti, D., Falcinella, C., Mulè, G., Mondatore, D., Tavelli, A., Vegni, E., Marchetti, G. and d'Arminio Monforte, A. (2021). Anxiety and depression symptoms after virological clearance of COVID‐19: a cross‐sectional study in Milan, Italy. Journal of Medical Virology, 93(2), pp.1175-1179.
A cross-sectional study which followed up patients hospitalised with Covid19 in Italy. Patients were required to have a history of documented clinical recovery and virological clearance (two consecutive negative PCR tests within 24-48 hours). After one to three months, 105 patients underwent a clinical examination, completed a Hospital Anxiety and Depression Scale (HADS) questionnaire, and underwent mini mental state examination to evaluate potential cognitive disorders. Ongoing physical, psychological and cognitive problems were commonly reported.
Townsend, L., Dyer, A.H., Jones, K., Dunne, J., Mooney, A., Gaffney, F., O'Connor, L., Leavy, D., O'Brien, K., Dowds, J. and Sugrue, J.A. (2020) Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. Plos one, 15(11), p.e0240784.
Outpatient appointments are offered to people with positive PCR tests at a post-Covid19 review clinic in Ireland. Those attending were invited to participate in this study if at least six weeks had elapsed since resolution of symptoms and/or hospital discharge. Of the 128 patients who were consecutively enrolled, 56% had been initially managed as inpatients and 45% as outpatients. Over half (52%) were healthcare workers. Almost one third of participants had not returned to work after a median follow-up of ten weeks, attributed by the authors to a high burden of fatigue.
Vaes, A.W., Machado, F.V., Meys, R., Delbressine, J.M., Goertz, Y.M., Van Herck, M., Houben-Wilke, S., Franssen, F.M., Vijlbrief, H., Spies, Y. and Van’t Hul, A.J. (2020) Care dependency in non-hospitalized patients with COVID-19. Journal of Clinical Medicine, 9(9), p.2946.
Data were obtained from 1,837 non-hospitalised patients recruited from two Long Covid Facebook groups and a website register in The Netherlands and Belgium. Around 11 weeks after symptom onset, participants reported an increased need for personal care when reflecting on changes in their condition before and after infection. Despite few needing help previously, almost one third considered themselves to be at least partially dependent on others at follow-up.
Varsavsky, T., Graham, M.S., Canas, L.S., Ganesh, S., Pujol, J.C., Sudre, C.H., Murray, B., Modat, M., Cardoso, M.J., Astley, C.M. and Drew, D.A. (2020) Detecting COVID-19 infection hotspots in England using large-scale self-reported data from a mobile application: a prospective, observational study. The Lancet Public Health.
In a follow-up to the preprint paper by Sudre et al. (2020), Varsavsky et al. (2021) report findings based on entries of more than 2.8 million users of the Covid Symptom Study (Zoe) app. Incidence of acute Covid19 in England was estimated based on positive PCR test results from a sample of 1,912 app users who had reported new Covid19 symptoms. They reported that only 40% of those displaying classic Covid19 symptoms went on to have a PCR test.
Venturelli, S., Benatti, S.V., Casati, M., Binda, F., Zuglian, G., Imeri, G., Conti, C., Biffi, A.M., Spada, S., Bondi, E. and Camera, G., (2021). Surviving COVID-19 in Bergamo Province: a post-acute outpatient re-evaluation. Epidemiology & Infection, 149, e32, pp.1-9.
767 patients discharged from the emergency department or inpatient wards of an Italian hospital, Covid19 patients underwent their first post-discharge multidisciplinary assessment 12 weeks later. More than half continued to experience ongoing symptoms, including 31% who exhibited post-traumatic psychological symptoms. D-dimer levels consistent with pulmonary thromboembolism were detected in 17% of people.
Vlachou, M., Drebes, A., Candilio, L., Weeraman, D., Mir, N., Murch, N., Davies, N. and Coghlan, J.G., (2021) Pulmonary thrombosis in Covid-19: before, during and after hospital admission. Journal of Thrombosis and Thrombolysis, pp.1-7.
39 people who had initially tested positive for Covid19 and experienced severe acute respiratory distress underwent computed tomography pulmonary angiography (CTPA), because of increasing oxygen and very elevated D-dimer. Pulmonary thrombosis was seen in 46.2%. Pulmonary embolism was observed even after recovery from acute Covid-19. Four patients were re-admitted after having recovered from Covid-19 pneumonia and been discharged, having tested Covdi19 positive at first review but negative at the time of PE diagnosis on their second admission one and four weeks later. It is suggested that the risk of clots forming in the blood vessels of the lungs continues up to four weeks after hospital discharge. As Pulmonary Embolism was not always associated with substantial lung involvement, it was hypothesised that inflammatory processes occurring elsewhere in the body may be responsible.
Wildwing, T. and Holt, N. (2021) The neurological symptoms of COVID-19: a systematic overview of systematic reviews, comparison with other neurological conditions and implications for healthcare services. Therapeutic Advances in Chronic Disease, 12, p.2040622320976979.
Wildwing and Holt (2021) reported a high-level overview of available literature relating to neurological symptoms of Covid19. In addition to life-threatening symptoms (such as those seen in Guillain Barré Syndrome and encephalitis), the authors suggest that other types of symptoms are reported over the longer-term. They observe that these patterns of symptoms appear to be similar to those of other neurological conditions such as Chronic Fatigue Syndrome (CFS) and Functional Neurological Disorder (FND).
Xiong, Q., Xu, M., Li, J., Liu, Y., Zhang, J., Xu, Y. and Dong, W., (2021) Clinical sequelae of COVID-19 survivors in Wuhan, China: a single-centre longitudinal study. Clinical Microbiology and Infection, 27(1), pp.89-95
A longitudinal study from Wuhan, China, illustrated the self-reported long-term sequelae of 538 people who had previously been hospitalised with acute Covid19. A telephone follow-up survey was carried out around 14 weeks after discharge, at which time half of the survivors reported ongoing symptoms.
Yeoh, Y.K., Zuo, T., Lui, G.C.Y., Zhang, F., Liu, Q., Li, A.Y., Chung, A.C., Cheung, C.P., Tso, E.Y., Fung, K.S. and Chan, V. (2021) Gut microbiota composition reflects disease severity and dysfunctional immune responses in patients with COVID-19. Gut.
This research team, based in Hong Kong, investigated the relationship between Covid19 disease severity and an imbalance of gut bacteria. Up to 30 days after clearance of the SARS-CoV-2 virus, concentrations of inflammatory markers in the blood were found to be associated with disruption of digestive system micro-organisms (as detected in faeces samples from 27 Covid19 positive patients when compared with those of people whose samples were obtained before the pandemic.
Yong, S.J., (2020) *PREPRINT* Long-Haul COVID-19: Putative Pathophysiology, Risk Factors, and Treatments.
A reviewed of the literature around Long Covid, aiming to address gaps relating to disease progression, risk factors, and potential treatments. Proposed mechanisms included unresolved inflammation (from viral persistence, chronic inflammation, autoimmunity, or gut dysbiosis) and long-term tissue damage in one or more physiological systems. Pharmaceutical treatment and exercise-based rehabilitation were also discussed. This paper has not yet been peer-reviewed.
NIHR Evidence is covered by the creative commons, CC-BY licence. Written content and infographics may be freely reproduced provided that suitable acknowledgement is made. Note, this licence excludes comments and images made by third parties, audiovisual content, and linked content on other websites.