This is a plain English summary of an original research article. The views expressed are those of the author(s) and reviewer(s) at the time of publication.
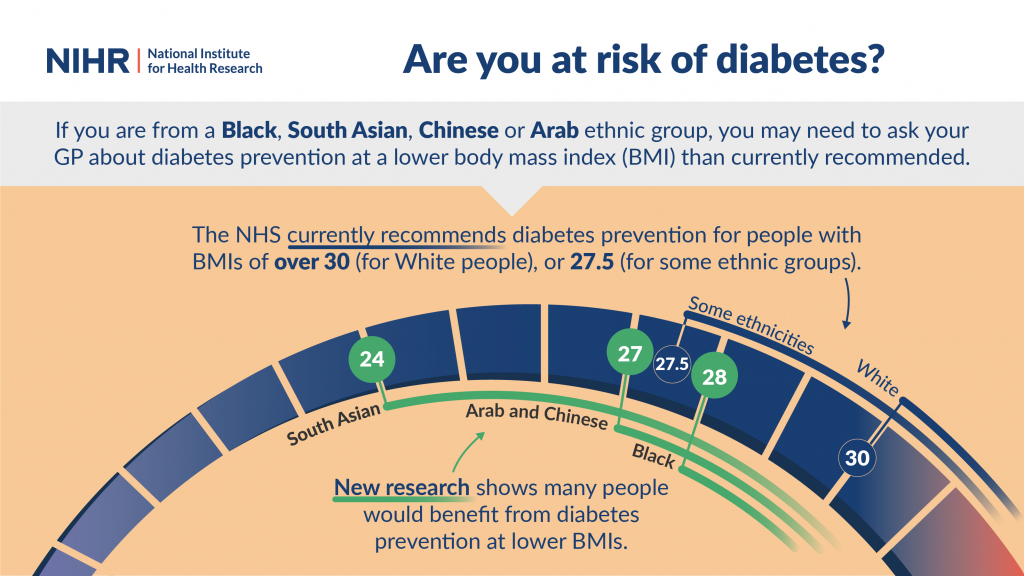
Interventions to prevent diabetes should be triggered at a different body mass index (BMI) for each ethnic group. New research found that some ethnic groups would benefit from prevention at a much lower BMI than is currently used.
Type 2 diabetes is related to body weight, and is much more common in people with obesity. In White populations, that means a BMI of 30. But this figure is not an appropriate guide in other ethnic groups.
Since 2004, the NHS has recommended diabetes prevention for people in some ethnic groups with BMIs of 27.5. However, this was based on limited evidence.
Now, researchers have detailed the BMI values which increase the risk of diabetes in different ethnic groups. For example, South Asian people with a BMI of 24 were found to be at risk of diabetes.
The study used data on more than a million people. It found that people of all ethnicities (other than White) were at risk of diabetes with a BMI lower than 30. In some groups, it was much lower. For example, the research suggests that people of Bangladeshi heritage could benefit from diabetes prevention even if they have a BMI of 21.
Please click here for a text description of this image
What’s the issue?
Around 1 in 4 people in the UK live with obesity. This increases their risk of type 2 diabetes, which can lead to kidney failure, loss of vision and other complications. But it is largely preventable through lifestyle changes such as weight management and physical activity. More information on type 2 diabetes is available on the NHS website.
BMI is calculated by dividing someone's height (in metres) by their weight (in kilograms). Obesity is typically defined as a BMI of 30 or more. Doctors tend to trigger actions to prevent type 2 diabetes at this BMI. Actions include advice on diet and physical activity, plus the use of a drug called metformin to improve control of blood sugar.
The definition of obesity (a BMI of 30+) was developed using data mostly from White populations. In 2004, the World Health Organization recommended lowering the BMI cut-off for Chinese and South Asian populations to 27.5. This was because people in these ethnic groups were developing type 2 diabetes at BMIs lower than 30. In response, the NHS issued guidance that a BMI of 27.5 should trigger diabetes prevention in Black, South Asian and Chinese people.
Now, a team of researchers has explored whether diabetes prevention should be started at still lower BMIs for people in some ethnic groups. They looked at a wider range of ethnicities than previous studies.
What’s new?
The team used electronic health records held by GPs and hospitals across England. They used data on almost 1.5 million adults with no previous or current diagnosis of type 2 diabetes. The records included people’s ethnicity and their BMI.
For the main analysis, the researchers considered participants in 5 groups: White (90.6%), South Asian (5.2%), Black (3.4%), Chinese (0.7%) and Arab (0.2%). Over a period of 6.5 years, almost 7% participants were diagnosed with type 2 diabetes.
The team measured how often White people with a BMI of 30 were diagnosed with type 2 diabetes. They then calculated the BMI in the other ethnic groups that indicated the same risk of diabetes. They adjusted for age and sex. BMI cut-offs were not affected by smoking or level of deprivation.
The study found that, in these ethnic groups, action to prevent type 2 diabetes is needed for people who have a BMI lower than 30.
Diabetes prevention is needed at or above a BMI of:
-
- 24 in South Asian populations
- 27 in Arab and Chinese populations
- 28 in Black populations.
A BMI of 24 would be considered healthy in a White population. But South Asian people with a BMI of 24 would benefit from diabetes prevention. This is much lower than the cut-off of 27.5 which is used currently.
The study was large enough for the team to look in more detail at South Asian and Black populations.
They found that, among different South Asian populations, diabetes prevention is needed at or above a BMI of:
-
- 21 in Bangladeshi populations
- 23 in Tamil and Sri Lankan populations
- 24 in Pakistani, Indian and Nepali populations.
Among Black populations, diabetes prevention is needed at BMI levels considered overweight (not obese) in White populations. Prevention is needed at or above a BMI of:
-
- 26 in Black Caribbean populations
- 27 in Black Other populations
- 29 in Black African populations
- just below 30 in Black British populations.
(The BMI figures shown here have been rounded).
Why is this important?
This is the first study to specify the BMI levels that indicate a risk of diabetes in different Arab, Black and South Asian populations. Current guidance comes from the National Institute for Health and Care Excellence (NICE) and NHS England. The guidance triggers action to prevent diabetes at higher BMI cut-offs than recommended by this study. This means that people from some ethnic minorities may be currently missing out on advice, tests, or referral to other services. South Asian people in particular could be at risk of developing diabetes at a BMI that is considered healthy in White people.
Triggering action sooner in these populations could prevent people from developing life-long diseases relating to obesity. This would improve their health and quality of life. People with type 2 diabetes require frequent health check-ups which can be resource heavy for both the NHS and the patient.
What’s next?
The study included people from specific ethnic groups. It excluded people from other ethnic groups and those who have mixed ethnicity. Further research is needed to explore BMI thresholds in these groups.
The reasons behind the study’s findings remain unclear. Genetics relating to body fat composition could play a role (for instance, Asian people typically have a higher percentage of body fat than White people with the same BMI). Lifestyle factors including diet and exercise are likely to be important. Or it could be due to a combination of lifestyle factors and genetics.
The researchers say that, if lifestyle is responsible, the BMI cut-offs could change with time. Future generations might have different lifestyles from their parents, which could affect their risk of obesity. However, if genetics are responsible, these cut-offs will remain lower than for the White population.
The researchers are expecting their finding to be reflected in the NICE guideline ‘Obesity: identification, assessment and management guidance’, when it is updated. To reflect the lower BMI threshold at which ethnic minority groups are in danger of developing type 2 diabetes. These thresholds are likely to be relevant for prevention of other diseases related to obesity, such as heart attacks and strokes.
In June 2021, GP practices were asked to produce a register of all patients living with obesity. The aim is to ensure that this group is offered support for weight loss. These findings suggest that more patients from some ethnic groups should be considered obese - and would benefit from intervention. Obesity registers may need to be updated as a result.
You may be interested to read
This summary is based on: Caleyachetty R, and others. Ethnicity-specific BMI cutoffs for obesity based on type 2 diabetes risk in England: a population-based cohort study. The Lancet Diabetes & Endocrinology 2021;9:419-426
The current guidelines the authors recommend be updated: National Institute for Health and Care Excellence (NICE). Obesity: identification, assessment and management. NICE guideline [CG189]. 2014
The enhanced service specification asking GP surgeries to record the BMI of registrants.
Funding: This study was funded by the NIHR under its Research for Patient Benefit programme.
Conflicts of Interest: The study authors declare no conflicts of interest.
Disclaimer: Summaries on NIHR Evidence are not a substitute for professional medical advice. They provide information about research which is funded or supported by the NIHR. Please note that the views expressed are those of the author(s) and reviewer(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Text description of the image: This image contains a semicircular scale of BMIs. On one side of the scale are the current research recommendations that say diabetes prevention at BMIs of 30, or 27.5. On the other side of the scale are the results of this new research, showing that diabetes prevention should start at lower BMIs for different ethnic groups. The text reads: "Are you at risk of diabetes? If you are from a Black, South Asian, Chinese or Arab ethnic group, you may need to ask your GP about diabetes prevention at a lower body mass index (BMI) than currently recommended. The NHS currently recommends diabetes prevention for people with BMIs of over 30 (for White people) or 27.5 (for some ethnic groups). New research shows many people would benefit from diabetes at lower BMIs."
NIHR Evidence is covered by the creative commons, CC-BY licence. Written content and infographics may be freely reproduced provided that suitable acknowledgement is made. Note, this licence excludes comments and images made by third parties, audiovisual content, and linked content on other websites.
