Vaccination is the most important thing we can do to protect ourselves and our children against ill health. Vaccines prevent up to 3 million deaths worldwide every year.
NHS: Why vaccination is safe and important
Vaccines protect individuals and society from infectious diseases. However, people vary in their acceptance; age, ethnicity, household income and other factors influence their willingness to be vaccinated. Research can identify ways to improve vaccine uptake in certain groups and reduce inequalities.
This Collection brings together examples of NIHR research on how to increase vaccine uptake. It explores how to engage and communicate effectively with different communities. It provides useful information for those commissioning and delivering vaccination services.
Introduction: why do we need vaccines?
Vaccines contain killed or weakened forms of viruses or bacteria (such as flu and polio), which train the immune system to fight off disease. They build immunity or resistance to infections. Vaccines also protect against some forms of cancer. For example, the human papillomavirus (HPV) vaccine protects against cancers of the cervix, anus, and genitals. The NHS offers people a wide range of vaccines from soon after birth to older age.
Diseases like smallpox, polio and tetanus used to kill or disable millions of people. Since vaccines were introduced, these diseases have either been eradicated or become very rare in the UK. Other diseases, such as measles and diphtheria, have been reduced by 99.9% since their vaccines were introduced. However, to be most effective, vaccination programmes depend on a large enough proportion of the public accepting the vaccine. When this happens, so-called herd immunity reduces the spread of a disease, meaning that both vaccinated and unvaccinated people are protected.
The uptake of vaccines is lower in certain communities and populations. This can put people at risk of ill health and widen health inequalities. For example, in the UK in 2021, only 2 in 3 Black Caribbean people over 40 had received a COVID-19 vaccine, compared with more than 9 in 10 White British people. Similarly, the UK Health Security Agency warned recently that teenagers could be at risk of rare but serious diseases (such as tetanus, diphtheria and polio) after a drop-off in vaccinations during the pandemic.
One of the aims of the NHS Long term Plan is to increase vaccine coverage in groups and areas with low uptake. This Collection addresses that aim.
How to engage communities

Understand the community’s needs
Understanding and responding to the specific needs of different communities helps build trust and overcome barriers to vaccination. Different groups will have different concerns that need to be addressed. For example, a survey of more than 1,200 parents of very young children was conducted before the COVID-19 vaccine was approved. One of the main concerns of parents was that the vaccine was being rushed through, with insufficient testing. This group needed a specific concern to be addressed in public health messages.
The same study found that people from black, Asian, Chinese, and mixed ethnic backgrounds were 3 times more likely to say they would refuse the vaccine than White British people. Those with lower household incomes were more likely to refuse the vaccine than households with higher incomes. The study concluded that, to prevent inequalities in vaccine uptake, services would need to understand people’s concerns (especially in groups with low vaccine coverage).
For example, some migrant communities have low vaccine uptake. Other researchers explored their needs and concerns in a review of 67 papers. They found that community advocates could increase vaccine uptake, possibly because they could deliver tailored messages that people trusted. Messages aligned to religious teachings on health were helpful.
Similarly, Gypsy, Traveller and Roma people have lower vaccine uptake. A study included more than 170 Gypsy, Roma and Traveller people in 5 workshops across the UK. Easier access to vaccines was found to be more important than addressing beliefs about vaccine safety or the need for vaccination. Participants said they would appreciate having a dedicated support officer in GP practices (such as a receptionist or administrator) who could deal with issues affecting their community. Administrators and clinicians could receive cultural competence training to help them understand the community’s needs. Health visitors were highly valued by these communities and could provide a bridge to mainstream health services for those who use them less often.
Deliver vaccines and information in community settings
The setting in which vaccines are delivered matters. For example, the review above found that migrants preferred familiar and local settings which require minimal travel, such as walk-in clinics at food banks, community centres, and charities.
Some pharmacies which provide drug (opioid) substitution therapies now promote flu vaccination alongside medication pick up. A campaign led by the Sheffield City Council Drug and Alcohol Action team, discussed in an NIHR Collection, led to a gradual increase in vaccination among people dependent on opioids.
A survey asked more than 2,000 people aged over 50 in England whether they had had, or intended to have, a COVID-19 booster vaccine. It found that 1 in 7 (14%) were undecided about having the vaccine; people in the undecided group were more likely than others to be from ethnic minority communities. Based on their findings, the researchers recommended hosting vaccination sessions in religious and other community venues. They emphasised the need to build trust in health systems, through culturally appropriate educational materials, addressing specific concerns about the vaccine, and tackling vaccine misinformation.
These findings were echoed in a report from the research group Collaboration for Change, which explored the views of ethnic minority groups on the COVID-19 vaccine. The report again recommended that vaccines be delivered in accessible locations within people’s communities, and stated that community organisations were well-placed to organise vaccination events. Some people were reassured by the presence of community members when being vaccinated. This helps to reinforce vaccination as a normal and important thing to do. Establishing this social acceptance of vaccination was identified as an effective way to increase vaccine uptake in a Wellcome Trust report.
Since the pandemic, the uptake of the HPV vaccine (normally given to girls and boys aged 12 to 13) has declined in the UK from 86% to 69%. One previously identified reason for low HPV vaccine uptake was a lack of information for students; school-based initiatives could address this. An NIHR-supported programme, called EDUCATE, was co-produced by young people and researchers from the University of Bristol and London School of Hygiene and Tropical Medicine. Programme resources (including films and exercises) aim to educate students about the HPV vaccine and its benefits, and could be delivered by teachers or community nurses. Research is underway to see whether the programme increases vaccine uptake.
Seize every opportunity to vaccinate
A study involving more than 250 pregnant women in the UK and 4 EU countries found that many women were unaware of the need for vaccination during pregnancy. Many said they had not received a recommendation to vaccinate from their doctors. This suggests that opportunities to promote vaccination among pregnant women are being lost. The researchers suggest that health professionals stress the importance of vaccination at regular appointments with pregnant women. They also recommend exploring the reasons why healthcare professionals may not be recommending vaccination.
This is in line with NICE recommendations on opportunistic vaccination, which suggest that healthcare professionals use every opportunity to identify people who have vaccines due. Clinicians could look at people’s vaccination records and offer those who are eligible a vaccine, book an appointment, or refer parents to school nurses or health visitors for their children’s vaccinations. If people refuse a vaccine, NICE recommends recording their reason; these reasons can be explored in future contacts to try and overcome barriers.
Suggestions for practice
- Community advocates and health visitors can increase vaccine uptake among migrant and travelling communities.
- Pharmacies, religious centres, and other community settings can reduce barriers. Â
- Children could learn about vaccines at school.
- Regular health appointments, such as check ups for pregnant women, are opportunities to encourage people to get vaccinated.
Effective Communication
Public health campaigns need to consider differences in the audience’s educational levels, religions, and cultural beliefs. They need to deliver the right message to the right group, via the right channel.

Emphasise the personal benefits of vaccines
Most people in the UK accepted the COVID-19 vaccine when it was offered, but some were hesitant. A study involving almost 19,000 people assessed different methods of communication. It found that stressing the personal benefits of the COVID-19 vaccine, rather than the benefits to the community, encouraged some people who were unsure about having the vaccine. Personal benefits included the prevention of serious illness and long COVID. Stressing these personal benefits could increase vaccine uptake across the population.
Monitor uptake to target specific groups
Monitoring vaccine uptake allows researchers to identify specific groups with low vaccine uptake, develop targeted campaigns for those groups, and engage with them about the reasons why they are hesitant.
When pregnant women are unvaccinated, both they and their child are at risk. Yet, nearly a quarter of women of reproductive age in England were not vaccinated against COVID-19 by February 2022.
Similarly, a study (involving more than 220,000 women) examined the uptake of pertussis and flu vaccines among pregnant women in England between 2010 to 2016. It showed that uptake was lower among younger women, women from ethnic minority groups, women living in areas of greater deprivation, London, and the North East. Tailoring public health messaging to resonate with these groups, through channels they are likely to use, could increase vaccine uptake.
Tackle misinformation
Misinformation (inaccurate information unintentionally presented as fact) and disinformation (deliberate spread of false information) have been linked with reduced intention to have a vaccine. Researchers analysed 34 studies on communication strategies to tackle vaccine misinformation. Their findings are summarised in the infographic below.
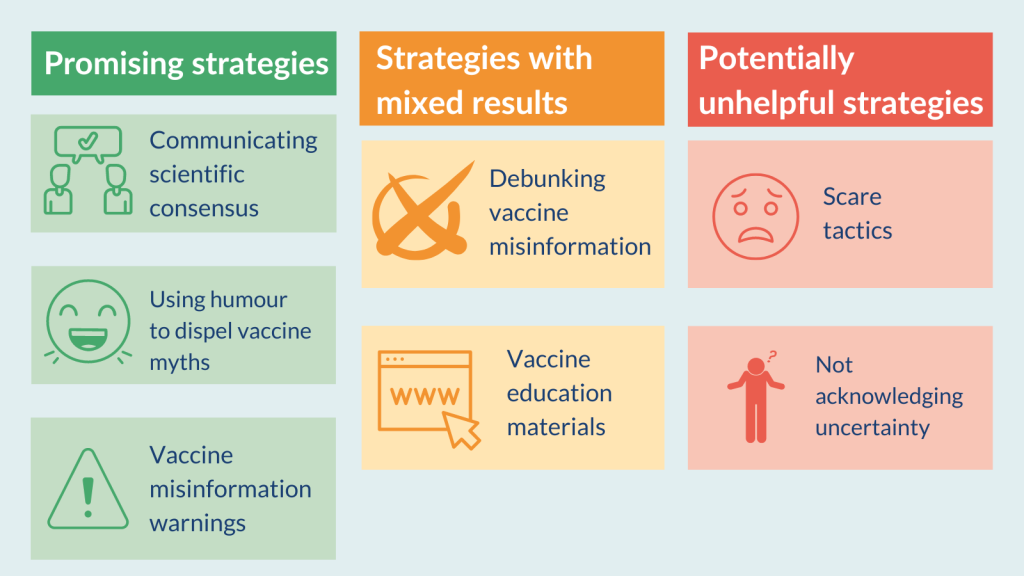
Communicating the scientific consensus that vaccines are safe and effective, using humour to dispel vaccine myths, and providing people with misinformation warnings (on Google search, for example) were promising strategies. Conversely, scare tactics (such as photos of children with symptoms of vaccine preventable diseases) could backfire and increase fears about vaccine side effects among some people. Not acknowledging scientific uncertainties made people less likely to have a vaccine. Attempting to debunk vaccine misinformation and providing education materials had mixed results.
The researchers say their findings could be used by public health communicators and policymakers to develop effective vaccination campaigns.
Use text messages and social media
Technology can help increase uptake and one of the most effective methods is simple: send phone and text reminders for vaccine appointments. As outlined in the Wellcome Trust report, Effective ways to increase vaccination rates, phone call reminders can increase attendance at vaccination appointments by 18%.
In a study of Gypsy, Roma and Traveller people’s views on vaccination (involving more than 170 people), participants said that they would appreciate flexible booking systems, using both text messages and letters. NICE recommends inviting both older and younger people for vaccines using their preferred method of communication: letter, phone, text, and email.
Social media can be a powerful tool to share public health messaging, especially when it includes videos. Many people who will not engage with written materials, will watch videos including public health messages. During the pandemic, the UK Government partnered with social media platforms including Snapchat, Reddit, TikTok and YouTube, to encourage people to get the vaccine. A study involving nearly 28,000 children and teenagers found that only half would have a COVID-19 vaccine. The researchers published vaccine education materials on social media, such as Tik Tok, to help young people engage via channels they already use.
Suggestions for practiceÂ
- Stress the personal benefits of vaccination, rather than benefits to the community; this was effective across several populations.
- Monitor vaccine uptake and tailor public health messages to resonate with groups with low uptake.
- Communicate the scientific consensus, use humour to dispel vaccine myths, and provide misinformation warnings.
- Text appointment reminders can increase attendance.
Conclusion
This Collection brings together some effective ways of engaging people about vaccination and communicating effectively. Research shows that listening to and understanding people’s concerns is at the heart of any effective strategy. Services need to make accessing vaccination as easy as possible and public health messages about vaccines need to be adapted and refined for specific audiences.
We hope the approaches outlined in this Collection will help services to deliver on one of the NHS Long Term plan's targets: to increase vaccine uptake where it is low and reduce health inequalities.
Author: Brendan Deeney, Science Writer, NIHR Evidence
How to cite this Collection: NIHR Evidence; Promoting vaccination: the right approach for the right group; July 2023; doi: 10.3310/nihrevidence_59296
Disclaimer: This Collection is based on research which is funded or supported by the NIHR. It is not a substitute for professional healthcare advice. Please note that views expressed are those of the author(s) and reviewer(s) at the time of publication. They do not necessarily reflect the views of the NHS, the NIHR or the Department of Health and Social Care.
NIHR Evidence is covered by the creative commons, CC-BY licence. Written content and infographics may be freely reproduced provided that suitable acknowledgement is made. Note, this licence excludes comments and images made by third parties, audiovisual content, and linked content on other websites.